|
|
|
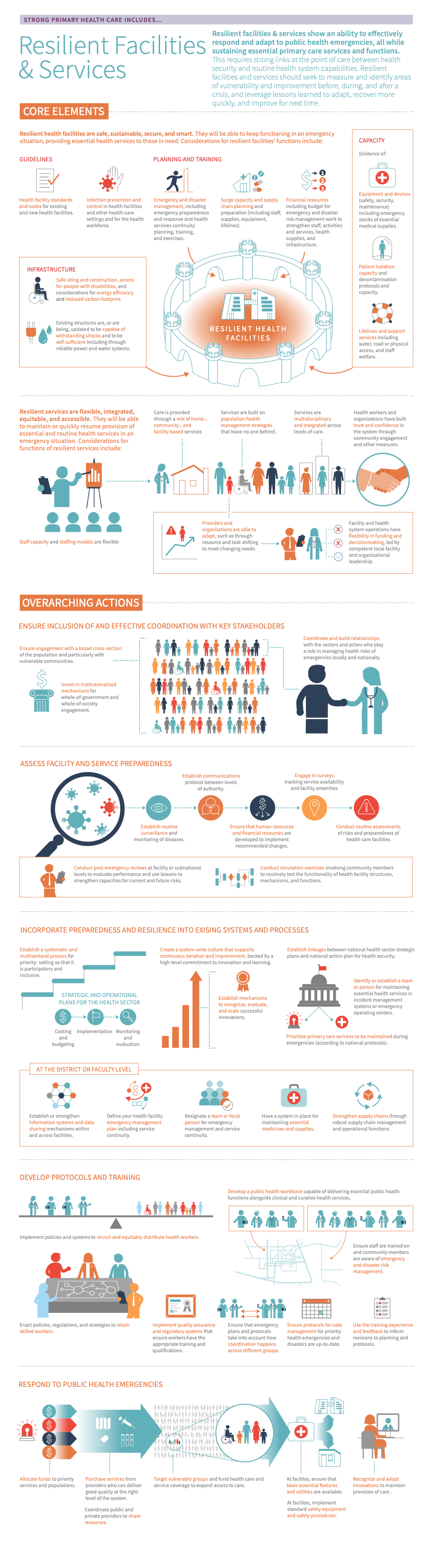
Strong PHC increases resiliency in facilities and services both in preparation for inevitable emergencies and in response to them.
All countries are vulnerable to emergencies or shocks that drastically affect the health system, such as earthquakes, disease outbreaks, conflicts, economic shocks, climate change, and pandemics. Resilient facilities and services refer to the existence of strong and sustainable linkages between Health security “The activities required, both proactive and reactive, to minimise the danger and impact of acute public health events that endanger people’s health across geographical regions and international boundaries.” and health system capabilities at the point of care.
Assessing service Preparedness “1. Activities and measures taken in advance to ensure effective response to the impact of hazards, including the issuance of timely and effective early warnings and the temporary evacuation of people and property from threatened locations (ISDR). 2. Pre-disaster activities, including an overall strategy, policies, and institutional and management structures that are geared to helping at-risk communities safeguard their lives and assets by being alert to hazards and taking appropriate action in the face of an imminent threat or the actual onset of a disaster (OCHA-WFP).” and Resilience “The ability of a system, community, or society exposed to hazards to resist, absorb, accommodate to, and recover from the effects of a hazard in a timely and efficient manner, including through the preservation and restoration of its essential basic structures and functions through risk management.” includes ensuring the presence of key inputs and measures to identify areas of vulnerability and opportunities for improvement in service delivery before, during, and after public health emergencies. This includes a focus on Emergency “An extraordinary situation in which people are unable to meet their basic survival needs, or there are serious and immediate threats to human life and well-being. Emergency interventions are required to save and preserve human lives and/or the environment. An emergency situation may arise as a result of a disaster, a cumulative process of neglect or environmental degradation, or when a disaster threatens and emergency measures have to be taken to prevent or at least limit the effects of the eventual impact. (UNDP)” and Disaster “A serious disruption of the functioning of a community or a society at any scale due to hazardous events interacting with conditions of exposure, vulnerability and capacity, leading to one or more of the following: human, material, economic and environmental losses and impacts.” risk management, comprehensive services and provider training enabling flexible and adaptive continuity of services and functions during emergencies, and the use of reviews and lessons learned to facilitate Recovery “The restoring or improving of livelihoods and health, as well as economic, physical, social, cultural and environmental assets, systems and activities, of a disaster-affected community or society, aligning with the principles of sustainable development and “build back better”, to avoid or reduce future disaster risk.” and strengthen capacities for current and future risks as keys to ensuring resilience. 12
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Before taking action, countries should first determine whether resilient facilities & services is an appropriate area of focus and where to target improvement efforts. Read on to learn how to use country data to:
- Make informed decisions about where to spend time and resources
- Track progress and communicate these updates to constituents or funders
- Gain new insights into long-standing trends or surprising gaps
Countries can measure their performance using the Vital Signs Profile (VSP). The VSP is a first-of-its-kind tool that helps stakeholders quickly diagnose the main strengths and weaknesses of primary health care in their country in a rigorous, standardized way. The second-generation Vital Signs Profile measures the essential elements of PHC across three main pillars: Capacity, Performance, and Impact. Organization of services is measured in the Management of Services and Population Health domain of the VSP (Performance Pillar).
If a country does not have a VSP, they can begin to focus improvement efforts using the subsections below, which address:
- Key indications
-
If your country does not have a VSP, the indications below may help you to start to identify whether resilient facilities & services is a relevant area for improvement:
- Information systems: There is little to no data on the current conditions of facilities within the health system and, specifically, on gaps at the facility level, such as measurements of service availability, readiness, and provision.
- Population health management: Disaster and emergency response protocols are outdated, do not exist, or do not incorporate input from a diverse set of stakeholders.
- Health infrastructure: Patients, providers, and facility staff are at risk of infection and disease due to factors such as contaminated water, food, or medical equipment; inadequate sharps and infectious waste disposal; or potential for unsafe blood transfusion.
- Organisation of services: All services are facility-based with no diversification into telehealth or community- or home-based services.
- Provider capacity: Providers are siloed within their specialties rather than working in multidisciplinary teams.
- Facility organisation and management: Facility management is weak.
- Availability of effective PHC services: Local integration between health care, public health services, and social sectors is weak or nonexistent.
- Health services: The health system has limited or no ability to maintain essential health services while responding to health systems shocks or public health emergencies.
- Policies and planning: There is limited or no up-to-date contingency planning for health services or health facility business continuity plans for emergencies in place, or those that exist lack dedicated budgets and funding, clearly defined roles and responsibilities, and accountability mechanisms.
- Key outcomes and impact
-
Countries that improve the resilience of facilities and services may achieve the following benefits or outcomes:
- Increased preparedness: Increased preparedness can help vulnerable communities safeguard their health, lives, and assets by being alert to hazards and ready to take appropriate action in the face of an imminent threat or the onset of a disaster or shock. 3
- Risk management: Risk management can help prevent the development of risks from disasters in the health system as well as reduce existing risks. It can also contribute to increased system resilience and reduced losses due to disasters. 4
- Increased resiliency: Resilient facilities can withstand or quickly recover from shocks while maintaining the capacity to continue providing essential care during emergencies, and can help communities recover more quickly as well. 5 As PHC is often the first point of contact between communities and the health system, maintaining surveillance, contact tracing, screening, risk communication, and vaccination can prevent a small-scale outbreak from becoming a larger, more disruptive event.
- Improved management and organisation, access, and equity: Many things that are necessary for resilience—decentralised decision-making, good management, robust supply chains, workforce with comprehensive skill sets, diverse methods of service delivery—are also essential to improving overall PHC. Therefore, focusing on resilience can simultaneously improve overall health system and facility management as well as organisation, access, and equity. 6
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Explore this page for a curated list of actions to improve the Resilience “The ability of a system, community, or society exposed to hazards to resist, absorb, accommodate to, and recover from the effects of a hazard in a timely and efficient manner, including through the preservation and restoration of its essential basic structures and functions through risk management.” of facilities and services, which embark on:
- An explanation of why the action is important for resilient facilities and services
- Descriptions of activities or interventions countries can implement to make their facilities and services more resilient
- Descriptions of the key drivers in the health system that should be improved to maximise the success or impact of actions
- Relevant case studies, tools, or resources that showcase what other countries around the world are doing to improve the resilience of their facilities and services as well as select tools and resources
Key actions:
-
Community engagement Community engagement is the inclusion of local health system users and community members in all aspects of health planning, provision, and governance. It is a central component of ensuring that the services delivered are tailored to population needs, priorities and values, which can be achieved through the involvement of communities in the design, financing, governance, and implementation of PHC. To ensure that the needs of all community members are met, it is important that community engagement efforts include representation from diverse members of the community. This may require multiple mediums for engagement, to best capture the needs and opinions of traditionally underrepresented community members. is an important aspect of preparedness, response, recovery, and resilience. 614 Primary care Primary care is “a key process in the health system that supports first-contact, accessible, continuous, comprehensive, and coordinated patient-focused care.” providers and staff can help increase patient and community trust in health services both before and during crises through thoughtful engagement. 4 Community and stakeholder engagements should occur throughout planning, risk assessment, implementation, review, and ongoing preparedness activities, which include facility emergency planning, facility surveys, and seeking input and funding. 6
Key activities
National and sub-national levels
- Ensure engagement with a broad cross-section of the population and particularly with vulnerable communities. Emergencies, disasters, and shocks can disproportionately affect more vulnerable populations including women, children, immigrants and refugees, elderly people, people with mental or physical disabilities, people with chronic diseases, and other individuals and communities with higher levels of risk. Planning and work should include perspectives and input from people in these populations to increase the likelihood of appropriately identifying and increasing the capacity to face s and vulnerabilities. 6
- Invest in institutionalised mechanisms for whole-of-government and whole-of-society engagement. Review existing mechanisms for whole-of-society action including expanding multisectoral approaches to health systems strengthening and management, community engagement and empowerment, and multi-stakeholder and participatory governance. Develop policy, legislative, and regulatory instruments to employ whole-of-government and whole-of-society (including private sector such as private health care providers) resources to support public health emergency preparedness, response, and efforts, including capacity-building for ongoing and future threats (see the policy & leadership module for more information).
District &/or facility level
- Coordinate and build relationships with the sectors and actors who play a role in managing health risks of emergencies locally and nationally: technical experts such as urban planners, civil engineers, hazardous facilities operators, climate information providers, animal health professionals, critical infrastructure managers (including energy, water, and sanitation), telecommunications and transport providers, pharmaceutical companies, and emergency services. 6 This key activity supports effective risk management and helps enable health services to continue functioning effectively in emergency contexts.
Individual &/or community level
- Collaborate with at-risk populations as well as the organisations and actors who play a role in meeting the needs of vulnerable populations. Health service providers have an important role in minimising the negative health outcomes associated with emergencies. Collaboration is essential to managing health risks for these populations and to developing and maintaining plans for continuing essential services in emergencies. Relevant stakeholders may include: 6
- community groups and members of vulnerable and at-risk populations;
- local, regional, and national government leaders and agencies;
- health system and services providers, including members of the ministry of health, representatives of health-related non-governmental organisations and private groups, primary care and other health care providers, and facility representatives; and
- other groups including academia and the research community, the media, the private sector, multinational companies, and international organisations
Related elements
Relevant tools & resources
- Karamagi et al., 2022: On the resilience of health systems: A methodological exploration across countries in the WHO African Region
- Mustafa et al., 2022: COVID-19 Preparedness “1. Activities and measures taken in advance to ensure effective response to the impact of hazards, including the issuance of timely and effective early warnings and the temporary evacuation of people and property from threatened locations (ISDR). 2. Pre-disaster activities, including an overall strategy, policies, and institutional and management structures that are geared to helping at-risk communities safeguard their lives and assets by being alert to hazards and taking appropriate action in the face of an imminent threat or the actual onset of a disaster (OCHA-WFP).” and Response Plans from 106 countries: a review from a health systems resilience perspective
- World Bank, 2022: Global Facility for Disaster “A serious disruption of the functioning of a community or a society at any scale due to hazardous events interacting with conditions of exposure, vulnerability and capacity, leading to one or more of the following: human, material, economic and environmental losses and impacts.” Reduction and Recovery “The restoring or improving of livelihoods and health, as well as economic, physical, social, cultural and environmental assets, systems and activities, of a disaster-affected community or society, aligning with the principles of sustainable development and “build back better”, to avoid or reduce future disaster risk.” annual report
-
Assessments are important to understand current facility and service preparedness and to prioritise the necessary infrastructure and operations changes. Assessments are essential to identify needs that can be prioritised and take place progressively over time. The tools and metrics described below can help with prioritisation.
Key activities
National and sub-national levels
- Establish routine surveillance and monitoring of diseases.
- Establish communications protocols between higher and lower levels of authority within the health system.
- Ensure that human resources and financial resources are available and prepared to implement the recommended changes. 78 These resources include financing for potentially considerable retrofitting of physical structures, maintenance and strengthening of critical systems and equipment, planning and conducting exercises, and revising emergency management plans based on training. Additionally, train and prepare the human resources who will staff the facilities.
- Address critical gaps in health system foundations. Use existing systems and processes to identify long-term health systems strengthening and emergency preparedness needs and inform resource allocation to address identified critical gaps. Similarly, leverage investments and attention on emergency preparedness and response to proliferating wider benefits to the health system through strengthened primary care and essential public health functions.
- Conduct routine surveillance activities, and use these learnings to facilitate recovery and strengthen future response efforts. Routinely reviewing health system operations through after-action reviews, operations reviews, routine disease surveillance, and health management information systems data collection can provide important information about system vulnerabilities, which can then be targeted for improvement prior to future shocks.
- Develop or strengthen national action plans for ; disaster risk reduction; emergency preparedness, response, and recovery; and incident management systems. If these plans and guidelines are already in place, ensure continuity between and accountability for plans across jurisdictions and the national/subnational level. Ideally, the plans should accommodate and complement one another. Additionally, emergency preparedness and response plans should be tested, reviewed, and revised as necessary on a regular basis. 3
District &/or facility level
- Use surveys to track service availability and facility amenities. Examples include the Service Availability and Readiness Assessment (SARA), Service Provision Assessments (SPA), or Service Delivery Indicators (SDI).
- Ensure risk assessments consider structural, non-structural, functionality, and preparedness of health care facilities on a routine basis.
- Conduct routine simulation exercises with community members to test the functionality of health facility structures, mechanisms, and functions for emergency management and service continuity under conditions.
- Conduct post-emergency reviews at the facility or subnational level to evaluate health facility and system performance in emergency management and service continuity under disaster conditions. Use the lessons learned to improve recovery and strengthen capacities for current and future risks.
- Conduct hospital and health centre safety evaluations at every health care facility, subnationally. Utilise data collection tools and metrics described below to inform these assessments. Use the findings of these assessments to improve the facility functions described in the Deep Dive section.
- At the facility level, put in place mechanisms to ensure the continuity of service functions in times of crisis. These mechanisms can include flexible funding for PHC, telehealth, reliable logistics management information systems, and reliable supply chains. If these mechanisms are lacking, make certain facilities know where to turn for support for continued service delivery in an emergency.
Related elements
- Policy & leadership
- Physical infrastructure
- Information & technology
- Service availability & readiness
Relevant tools & resources
- Assessment tool: Safe Hospitals Checklist
- Use the Safe Hospitals Checklist, which applies to health facilities and other levels of health care, to obtain a rating of the structural and nonstructural safety and the emergency and disaster management capacity of a health facility.
- Assessment tool: WHO Harmonised Health Facility Assessment
- The Harmonised Health Facility Assessment (HHFA) is a comprehensive health facility survey tool for countries assessing the availability of health facility services as well as the capacities of facilities to provide services at required standards of quality.
- More details and downloadable guidance and tools for adapting, planning, and implementing a Harmonised Health Facility Assessment can be found in the Harmonised Health Facility Assessment resource package.
-
Ensuring effective planning and preparedness work takes place is a critical action to establishing a baseline level of emergency preparedness. Incorporating preparedness and resilience into existing systems and processes involves a range of stakeholders and actions at health system, district, and facility levels can ensure effective institutionalisation of this work.
Key activities
National and sub-national levels
- Establish a systematic and multisectoral process for priority-setting that is participatory and inclusive.
- Translate priorities into strategic and operational plans for the health system. Include costing and budgeting, implementation, and ongoing monitoring and evaluation.
- Create a system-wide culture that supports continuous iteration and improvement backed by a high-level commitment to innovation and learning.
- Establish mechanisms to recognize, evaluate, and scale successful innovations beyond pilot testing, and systematically share learnings across stakeholders.
- Establish linkages between national health system strategic plans and national action plan for Seek synergies in activities, budgets, and monitoring and evaluation, and identify areas that require focused attention from the health security or health systems sides. Also, link the national health sector strategic plan and disease-specific plans such as HIV, tuberculosis, malaria, and those relating to specific population groups including ethnic minorities, women and children, elderly, refugees, and vulnerable and marginalised communities.
- Identify or establish a team or focal person for maintaining essential health services in incident management systems or emergency operating centres.
- Establish or strengthen information systems and data sharing mechanisms within and across facilities and sectors at different levels. Ensure interoperability of information systems between clinical, public health, and veterinary sectors.
District &/or facility level
- Define your health facility emergency management plan, including service continuity. Identify a source of funding or a budget line.
- Designate a team or focal person for emergency management and service continuity.
- Prioritise primary care services to be maintained during emergencies according to national protocols.
- Create a system for maintaining essential medicines and supplies.
- Strengthen supply chains through robust supply chain management and operational functions, such as appropriate financing, performance management, and risk management. Ensure supply chains, prepositioned stocks, and essential medical products to enable service delivery in various settings such as the community, at home, through digital platforms, and in facilities.
Related elements
Relevant tools & resources
- Mansour et al., 2022: Health systems resilience in fragile and shock-prone settings through the prism of gender equity and justice: implications for research, policy and practice
- WHO, 2021: Fostering resilience through integrated health system strengthening: technical meeting report
- WHO, 2021: Building health systems resilience for universal health coverage and health security during the COVID-19 pandemic and beyond: WHO position paper
-
Developing protocols, and conducting training for staff, managers, providers, and the community will help ensure that people are more prepared to respond appropriately during an emergency, so facilities can continue providing services.
Key activities
National and sub-national levels
- Implement policies and systems to recruit and equitably distribute health workers, particularly in rural or marginalised communities. Across all areas of service delivery, train the health workforce with a public health orientation.
- Enact policies, regulations, and strategies to retain skilled workers, such as supportive supervision, continuing professional development, and appropriate remuneration.
- Implement quality assurance and regulatory systems that ensure workers have the appropriate training and qualifications, that workforce records are maintained, and that appropriate measures are taken to ensure workers meet established standards.
- Develop a public health workforce capable of delivering context-specific essential public health functions (including all-hazards emergency management and International Health Regulations [2005]) alongside clinical and curative health services.
District &/or facility level
- Ensure protocols for case management during priority health emergencies and disasters are up-to-date.
- Ensure staff are trained in and community members are aware of protocols for emergency and disaster risk management (including prevention, preparedness, response, and recovery) and service continuity.
- Ensure that emergency plans and protocols include coordination across different groups including women, children, immigrants and refugees, elderly, people with mental or physical disabilities, people with chronic diseases, and other individuals and communities with higher levels of risk. To the extent possible, create opportunities for cross-group engagement and coordination as part of ongoing training and work.
- Use training experiences and feedback to revise planning and protocols. Continue to practice and update plans and protocols periodically.
Related elements
Relevant tools & resources
- WHO, 2021. Health service continuity planning for public health emergencies: a handbook for health facilities. Interim version for field testing.
- WHO, 2021. Health Systems
Resilience
“The ability of a system, community, or society exposed to hazards to resist, absorb, accommodate to, and recover from the effects of a hazard in a timely and efficient manner, including through the preservation and restoration of its essential basic structures and functions through risk management.”
Simulation Exercises.
-
Health facilities and the PHC services PHC services refer to any intervention, procedure, regimen, or process that providers use to respond to the needs and demands of their patient population at the primary care level. Because of PHC’s community-facing orientation, services can be provided virtually or face-to-face in homes, communities, or PHC centres. Depending on the context, services may be provided by public or private providers. they provide are of critical importance in a health system emergency. Resilient facilities and services should be able to maintain or quickly return to providing essential and routine health services and to help with recovery. The overall aim of resilient facilities and services is “protect[ing] human life and produc[ing] good health outcomes for all during a crisis and in its aftermath.” 10
Key activities
National and sub-national levels
- Allocate funds to priority services and populations. Flexible health financing arrangements are critical for facilitating essential health services, especially during emergency situations. This flexibility ensures financial protection from catastrophic health expenditure for population members and mitigation of demand-side issues for services such as reduced uptake of essential health services due to affordability. It can also enable timely critical services such as surveillance, testing, contact tracing, prophylaxis, treatment, vaccination, and follow-up.
- Purchase services from providers who can deliver good quality at the right level of the system.
- Target vulnerable groups and fund health care and service coverage to expand access to care.
- Recognize and adopt innovations such as digital platforms and telehealth to maintain the provision of care when the health system is under stress.
- Coordinate public and private providers to share resources, such as workers and supplies.
District &/or facility level
- Ensure that essential features and utilities are available at facilities; see Deep Dive for more on these essential features.
- Implement standard safety equipment and safety procedures at facilities.
- Maintain continuity of services at the facility and community levels through task shifting and flexibility of services.
Related elements
Relevant tools & resources
- OECD, 2021: Strengthening the frontline: How primary health care helps health systems adapt during the COVID 19 pandemic
- PHCPI, 2021: PHC COVID-19 guidance on maintaining access to routine and essential services and surveillance and response
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Understanding and identifying the drivers of health systems performance--referred to here as “related elements”--is an integral part of improvement efforts. We define related elements as the factors in a health system that have the potential to impact, whether positive or negative, the resilience of facilities and services. Explore this section to learn about the different elements in a health system that should be improved or prioritized to maximize the success of actions described in the “take action” section.
While there are many complex factors in a health system that can impact the resilience of facilities and services, some of the major drivers are listed below. To aid in the prioritization process, we group the ‘related elements’ into:
Upstream elements
We define “upstream elements” as the factors in a health system that have the potential to make the biggest impact, whether positive or negative, on the resilience of health services.
- Adjustment to population health needs
-
Without frequent, evidence-based, and locally-driven priority setting, appropriately understanding which services should be maintained as essential during public health emergencies is a major challenge. Additionally, a lack of innovation and continual learning throughout the health system can interfere with the identification of new strategies for building greater resilience in existing and new PHC structures.
- Purchasing & payment systems
-
Purchasing and payment systems that are fragmented or inefficient can limit the flexibility necessary to adapt to providing essential routine and recovery services in an emergency.
- Physical infrastructure
-
Lack of appropriate physical infrastructure, established before an emergency, can impede a facility’s ability to rapidly respond to and maintain care during times of emergencies and endanger providers and staff.
- Medicines & supplies
-
Shortages or insufficient stocks of medicines and supplies to maintain operations and function during a health emergency can lead to delays in the ability to provide essential or routine health services.
- Health Workforce
-
A PHC system with an inadequate workforce or a workforce not prepared with the necessary skills and precautions needed in emergencies will not be able to provide the necessary services to meet the needs of its population.
- Information & technology
-
Without robust information, communication, and surveillance systems, the health system will struggle to maintain facility operations and essential functions during an emergency.
Complementary elements
We define “complementary elements” as the factors in a health system that have the potential to make an impact, whether positive or negative, on the resilience of facilities and services. However, we consider these drivers as complementary to, but not essential to performance in this area.
- Continuity
-
When facilities lack systems for informational and relational continuity of care, it increases the likelihood that patient information will not transfer effectively and means patients are less likely to have a point of access to the health system during a health emergency.
- Organisation of Services
-
When facilities are without adequate organisation of services, patients will not readily understand where and how services are provided. Further, facilities and providers will lack clear directives and roles during emergencies.
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Countries seeking to improve the resilience of facilities and services can pursue a wide array of potential improvement pathways. The short case studies below highlight promising and innovative approaches that countries around the world have taken to improve.
PHCPI-authored cases were developed via an examination of the existing literature. Some also feature key learnings from in-country experts.
- East Asia & the Pacific
- Europe & Central Asia
-
- Multiple countries: Assessing the resilience of health systems in Europe
- Latin America & the Caribbean
- Middle East & North Africa
- North America
- South Asia
- Sub-Saharan Africa
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Building consensus on what resilient facilities and services look like and key strategies to fix gaps is an important step in the improvement process.
Below, we define some of the characteristics of resilient facilities and services in greater detail:
-
“Not all emergencies can be predicted, but they can be prepared for.”
Dr Tedros Adhanom Ghebreyesus, Director-General, World Health Organisation 3All countries are vulnerable to emergencies or shocks of one sort or another. The same health system emergency–such as an earthquake, disease outbreak, conflict, economic shock, climate change, or pandemic–can occur with the same intensity in two countries or two communities. However, the extent of the damage to individual health, infrastructure, or health services may vary greatly depending on the communities’ vulnerability, , and . 9 Resilient facilities and services refer to the existence of strong and sustainable linkages between and health system capabilities at the point of care.
According to the USAID Blueprint for Global Health Resilience “The ability of a system, community, or society exposed to hazards to resist, absorb, accommodate to, and recover from the effects of a hazard in a timely and efficient manner, including through the preservation and restoration of its essential basic structures and functions through risk management.” , “health resilience is necessary to mitigate against the country and global shocks and stressors (both health and non-health). A prerequisite for health resilience is accessible primary health care.” 5 PHC is a patient’s first point of contact with the health system and should lead to trusting, respectful relationships and services that meet local needs and expectations. PHC collects local data that provide essential surveillance knowledge to all levels of the system, making strong PHC a core input to resilient facilities and services across the system. 7
During times of crisis, resilient facilities and services are essential for directly responding to the crisis, maintaining routine and essential services, and reducing the burden on tertiary facilities. 20 The COVID-19 pandemic has highlighted the importance of PHC for maintaining essential services during emergencies. Countries reported more than half of essential services were disrupted in 2020, on average, with ongoing disruptions continuing through 2021. 21
During emergencies, the ability of health services to continue functioning relies on key factors:
- That health services are housed in safe and secure facilities that are prepared for emergencies and capable of resisting exposures and forces from all types of s,
- That medical equipment is protected from damage and in working order,
- That community infrastructure and critical services, including water and power, continue to be available to support health services, and
- That health personnel can provide medical assistance in safe and secure settings when they are most needed. 9
Safe and secure facilities allow the maintenance of essential and routine health services in emergencies, supporting response and . 3
-
Resilient health facilities will be able to function in an emergency situation, providing essential health services to those in need. Considerations for resilient facilities’ functions include:
- Guidelines
- Consideration(s)
- There are standards and codes for existing and new health facilities.
- Infection prevention and control (in health facilities, in other health-care settings, and for the health workforce) exists
- Supporting resource(s)
- WHO, 2015: Comprehensive safe hospital framework
- Consideration(s)
- Infrastructure
- Consideration(s)
- The system prioritises safe siting and construction, universal design (e.g. access for people with disabilities), and considerations for energy efficiency and reduced carbon footprint.
- Existing structures are, or are being, updated to be capable of withstanding shocks and to be self-sufficient, including having reliable power and water systems.
- There is a focus on health facility security.
- Supporting resource(s)
- PHCPI, 2022: Physical infrastructure module
- WHO, 2022: Health systems for health security framework
- World Bank, 2021: Frontline: Preparing Healthcare Systems for Shocks from Disasters to Pandemics report
- Consideration(s)
- Planning and training
- Consideration(s)
- and management–including emergency and response and health services continuity planning, training, and exercises–is ongoing.
- There is surge capacity and supply chain planning and preparation (including staff, supplies, equipment, and lifelines).
- Financial resources exist, including budgets for emergency and disaster risk management work to strengthen staff, activities, and services; health supplies; and infrastructure.
- Supporting resource(s)
- PHCPI, 2022: Health workforce and Purchasing & payment systems modules
- WHO, 2021: Health service continuity planning for public health emergencies: a handbook for health facilities handbook
- World Bank, 2021: Frontline: Preparing Healthcare Systems for Shocks from Disasters to Pandemics report
- WHO, 2019: Health emergency and disaster risk management framework
- Consideration(s)
- Capacity
- Consideration(s)
- There is sufficient equipment and devices (safety, security, maintenance) and maintain emergency stocks of essential medical supplies.
- Patient isolation capacity exists.
- There are decontamination protocols and capacity.
- Lifelines and support services–including water, road or physical access, and staff welfare–are ensured.
- Supporting resource(s)
- PHCPI, 2022: Medicines & supplies and Information & technology modules
- Consideration(s)
- Guidelines
-
Resilient health facilities will be able to maintain or quickly resume the provision of essential and routine health services in an emergency situation. Considerations for functions of resilient services include: 4
- Staff capacity and staffing models are flexible (such as cross-training for comprehensive care) to enable rapid changes in deployment as health needs shift.
- Supporting resource(s)
- PHCPI, 2022: Management of services, Access, and Service availability & readiness modules
- Supporting resource(s)
- Care is provided through a mix of home-, community-, and facility-based services and providers to maximise opportunities to interact with the population and enable flexible care delivery depending on the emergency.
- Supporting resource(s)
- PHCPI, 2022: Access & availability and Population health management modules
- Supporting resource(s)
- Services are built on population health management strategies that leave no one behind.
- Supporting resource(s)
- PHCPI, 2022: Population health management module
- Supporting resource(s)
- Services are multidisciplinary and integrated across levels of care.
- Quality of care delivery is prioritised in maintaining essential and routine health services.
- Supporting resource(s)
- PHCPI, 2022: Primary care Primary care is “a key process in the health system that supports first-contact, accessible, continuous, comprehensive, and coordinated patient-focused care.” functions module
- WHO, 2021: Technical package on quality of care in fragile, conflict-affected, and vulnerable settings
- Supporting resource(s)
- Providers and organisations are able to adapt (e.g. through resource and task shifting to meet changing needs). There is local decision-making authority.
- Supporting resource(s)
- PHCPI, 2022: Management of services and Adjustment to population health needs modules
- Supporting resource(s)
- Providers and organisations have built trust and confidence in the system through community engagement and other measures.
- Supporting resource(s)
- PHCPI, 2022: Population health management module
- Supporting resource(s)
- Facility and health system operations have flexibility in funding and decision-making, led by competent local facility and organisational leadership.
- Supporting resource(s)
- PHCPI, 2022: Financing and Management of services modules
- Supporting resource(s)
- Staff capacity and staffing models are flexible (such as cross-training for comprehensive care) to enable rapid changes in deployment as health needs shift.
-
A single emergency or shock can severely impede the progress of primary health care and other sectors. 3 Increasing the resilience of facilities and services involves building capacity at three different levels:
Absorptive capacity
- Absorptive capacity involves taking preventative measures where possible in order to avoid or minimise negative impacts from health system shocks, emergencies, or disasters. The goal of absorptive capacity is to maintain health system stability. 5
- Examples include:
- Task-shifting or task-sharing in order to align health care workers with pressing needs. 5
- Developing memoranda of understanding between health facilities for coordination during emergencies. 25
Adaptive capacity
- Adaptive capacity involves developing approaches to respond to change. It is a health system’s (or health facility’s) ability to improve its overall performance while also being able to make ongoing adjustments. 5
- Examples include:
- Innovating and using digital platforms and tools during COVID-19 to conduct training and supportive supervision.
- Ensuring protected funding for facility improvements even (or especially) during times of calm.
Transformative capacity
- Transformative capacity involves building and leveraging an enabling environment that supports systemic change. This is a health system’s ability to address ongoing vulnerabilities or contextual factors that impact a system’s performance or a population’s health outcomes by making fundamental changes. 5
- Examples include:
- Establishing or formalising arrangements such as memoranda of understanding between public and private providers to share resources such as workers and supplies in times of crisis. 5
Developing these capacities must be undertaken through stakeholder engagement and be based on data, steps which are explored in more detail in the take action section of the module.
-
- Disaster “A serious disruption of the functioning of a community or a society at any scale due to hazardous events interacting with conditions of exposure, vulnerability and capacity, leading to one or more of the following: human, material, economic and environmental losses and impacts.” : “A serious disruption of the functioning of a community or a society at any scale due to hazardous events interacting with conditions of exposure, vulnerability and capacity, leading to one or more of the following: human, material, economic and environmental losses and impacts.” 26
- Emergency “An extraordinary situation in which people are unable to meet their basic survival needs, or there are serious and immediate threats to human life and well-being. Emergency interventions are required to save and preserve human lives and/or the environment. An emergency situation may arise as a result of a disaster, a cumulative process of neglect or environmental degradation, or when a disaster threatens and emergency measures have to be taken to prevent or at least limit the effects of the eventual impact. (UNDP)” : “An extraordinary situation in which people are unable to meet their basic survival needs, or there are serious and immediate threats to human life and well-being. Emergency “An extraordinary situation in which people are unable to meet their basic survival needs, or there are serious and immediate threats to human life and well-being. Emergency interventions are required to save and preserve human lives and/or the environment. An emergency situation may arise as a result of a disaster, a cumulative process of neglect or environmental degradation, or when a disaster threatens and emergency measures have to be taken to prevent or at least limit the effects of the eventual impact. (UNDP)” interventions are required to save and preserve human lives and/or the environment. An emergency situation may arise as a result of a disaster, a cumulative process of neglect or environmental degradation, or when a disaster threatens and emergency measures have to be taken to prevent or at least limit the effects of the eventual impact. (UNDP)” 27
- Hazard “A process, phenomenon or human activity that may cause loss of life, injury or other health impacts, property damage, social and economic disruption or environmental degradation.” : “A process, phenomenon or human activity that may cause loss of life, injury or other health impacts, property damage, social and economic disruption or environmental degradation.” 26
- Health security “The activities required, both proactive and reactive, to minimise the danger and impact of acute public health events that endanger people’s health across geographical regions and international boundaries.” : “The activities required, both proactive and reactive, to minimise the danger and impact of acute public health events that endanger people’s health across geographical regions and international boundaries.” 28
- Preparedness “1. Activities and measures taken in advance to ensure effective response to the impact of hazards, including the issuance of timely and effective early warnings and the temporary evacuation of people and property from threatened locations (ISDR). 2. Pre-disaster activities, including an overall strategy, policies, and institutional and management structures that are geared to helping at-risk communities safeguard their lives and assets by being alert to hazards and taking appropriate action in the face of an imminent threat or the actual onset of a disaster (OCHA-WFP).” : “1. Activities and measures taken in advance to ensure effective response to the impact of hazards, including the issuance of timely and effective early warnings and the temporary evacuation of people and property from threatened locations (ISDR). 2. Pre-disaster activities, including an overall strategy, policies, and institutional and management structures that are geared to helping at-risk communities safeguard their lives and assets by being alert to hazards and taking appropriate action in the face of an imminent threat or the actual onset of a disaster (OCHA-WFP).” 8
- Recovery “The restoring or improving of livelihoods and health, as well as economic, physical, social, cultural and environmental assets, systems and activities, of a disaster-affected community or society, aligning with the principles of sustainable development and “build back better”, to avoid or reduce future disaster risk.” : “The restoring or improving of livelihoods and health, as well as economic, physical, social, cultural and environmental assets, systems and activities, of a disaster-affected community or society, aligning with the principles of sustainable development and “build back better”, to avoid or reduce future disaster risk.” 26
-
Resilience
“The ability of a system, community, or society exposed to hazards to resist, absorb, accommodate to, and recover from the effects of a hazard in a timely and efficient manner, including through the preservation and restoration of its essential basic structures and functions through risk management.”
: “The ability of a system, community, or society exposed to hazards to resist, absorb, accommodate to, and recover from the effects of a hazard in a timely and efficient manner, including through the preservation and restoration of its essential basic structures and functions through risk management.” 26
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
References:
- WHO, UNICEF. Internal working draft: Primary health care performance: measurement for improvement- technical specifications. WHO; 2021 Oct.
- Armstrong, M. & Baron, A. (1998), Performance Management Handbook, IPM, London [Internet]. [cited 2019 Jan 30]. Available from: http://www.sciepub.com/reference/151290
- WHO. Health Emergency and Disaster Risk Management Framework. Geneva: World Health Organization; 2019.
- Kruk ME, Ling EJ, Bitton A, Cammett M, Cavanaugh K, Chopra M, et al. Building resilient health systems: a proposal for a resilience index. BMJ. 2017 May 23;357:j2323.
- USAID. BLUEPRINT FOR GLOBAL HEALTH RESILIENCE. USAID; 2021 Jun.
- WHO. Building health systems resilience for universal health coverage and health security during the COVID-19 pandemic and beyond: WHO position paper. Geneva: World Health Organization; 2021.
- WHO. Comprehensive safe hospital framework. Geneva: World Health Organization; 2015.
- Affun-Adegbulu C, Ricarte B, Van Belle S, Van Damme W, van de Pas R, van De Put W. Primary health care and Health Emergencies. Geneva: World Health Organization; 2018.
- WHO, PAHO. Hospital safety index: guide for evaluators. World Health Organization; 2015.
- WHO. Health systems for health security: a framework for developing capacities for international health regulations, and components in health systems and other sectors that work in synergy to meet the demands imposed by health emergencies. Geneva: World Health Organization; 2021.
- Nuevo CE, Yap ME, Boxshall M, Ravishankar N. IMPLEMENTING UHC IN THE PHILIPPINES: IS THE GLASS HALF FULL OR HALF EMPTY? [Internet]. P4H Social Health Protection Network. 2021 [cited 2022 Feb 13]. Available from: https://p4h.world/en/blog/IMPLEMENTING-UHC-IN-THE-PHILIPPINES/IS-THE-GLASS-HALF-FULL-OR-HALF-EMPTY%3F
- Yap MEC, Carpio LPD, Ong MM, Aposto VC. Development of a Competency Certification Framework for Primary Care Providers in the Context of Universal Health Care in the Philippines. ThinkWell Global; 2019 Dec.
- Liwanag HJ, Wyss K. What conditions enable decentralization to improve the health system? Qualitative analysis of perspectives on decision space after 25 years of devolution in the Philippines. PLoS ONE. 2018 Nov 5;13(11):e0206809.
- Casamina C, Lee C, Reyes R. Medical school hotline: tropical cyclone Haiyan/Yolanda medical relief mission: perspectives of John A. Burns School of Medicine 2nd year medical students. Hawaii J Med Public Health. 2015 May;74(5):176–8.
- Salazar MA, Pesigan A, Law R, Winkler V. Post-disaster health impact of natural hazards in the Philippines in 2013. Glob Health Action. 2016 May 17;9:31320.
- Salazar MA, Law R, Pesigan A, Winkler V. Health consequences of typhoon haiyan in the eastern visayas region using a syndromic surveillance database. PLoS Curr Influenza. 2017 Feb 6;9.
- Sebastian MMG. INVESTING IN PPPS FOR HEALTH [Internet]. Republic of the Philippines Public-Private Partnership Center. [cited 2022 Feb 13]. Available from: https://ppp.gov.ph/ppp-sectors/
- Law R. Resilient Health Systems Now More Than Ever [Internet]. Health Care Without Harm. 2020 [cited 2021 Dec 13]. Available from: https://www.noharm-europe.org/resilienthealthsystems
- Philippines Department of Health. National Disaster Resilience Month [Internet]. 2021 [cited 2022 Feb 13]. Available from: https://dilg.gov.ph/events/National-Disaster-Resilience-Month/667
- Rentschler J, Klaiber C, Tariverdi M, Desjonqueres C, Mercadante J. Frontline : Preparing Healthcare Systems for Shocks from Disasters to Pandemics. World Bank, Washington, DC; 2021 Apr.
- WHO. Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic. World Health Organization; 2021 Apr.
- WHO. Health service continuity planning for public health emergencies: A handbook for health facilities. World Health Organization; 2021.
- WHO. Quality of care in fragile, conflict-affected and vulnerable settings: taking action [Internet]. World Health Organization; 2020 Dec [cited 2021 Apr 5]. Available from: https://www.who.int/publications/i/item/9789240015203
- WHO. Quality of care in fragile, conflict-affected and vulnerable settings: tools and resources compendium. Geneva: World Health Organization; 2021 Jan.
- Meyer D, Bishai D, Ravi SJ, Rashid H, Mahmood SS, Toner E, et al. A checklist to improve health system resilience to infectious disease outbreaks and natural hazards. BMJ Glob Health. 2020 Aug;5(8).
- United Nations Office for Disaster Risk Reduction. United Nations Office for Disaster Risk Reduction: Terminology [Internet]. United Nations Office for Disaster Risk Reduction. 2017 [cited 2021 Dec 13]. Available from: https://www.undrr.org/terminology
- HealthAction in Crises. WORDS ARE IMPORTANT. World Health Organization; 2003 Oct.
- WHO. Health security [Internet]. World Health Organization. [cited 2021 Dec 13]. Available from: https://www.who.int/health-topics/health-security#tab=tab_1
