|
|
|
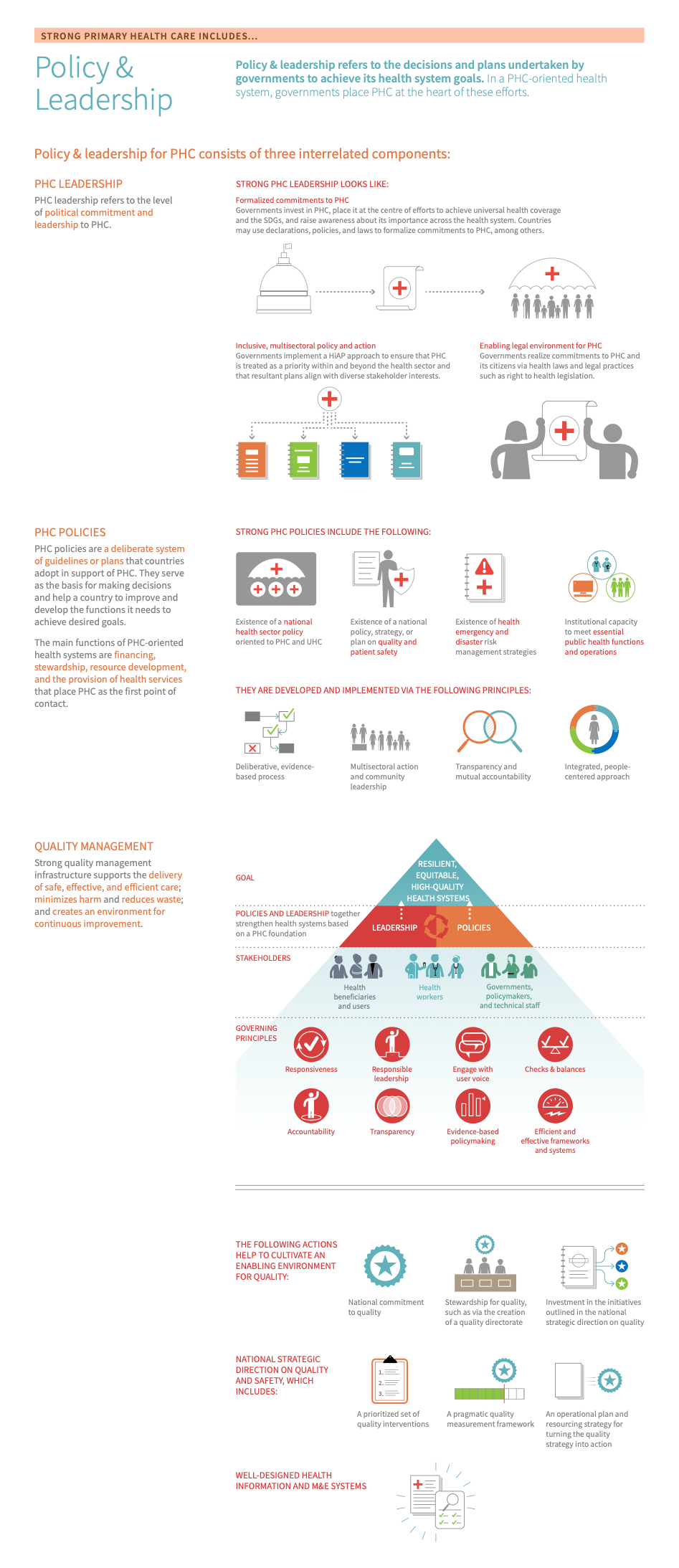
Policy & leadership refers to the decisions and plans undertaken by governments to achieve its health system goals. In a PHC-oriented health system, governments place PHC at the heart of these efforts. Thus, policy & leadership is the foundation of strong PHC because it creates the mechanisms by which PHC works, including financing, inputs, service delivery, quality management, and measurement. 12
Policy & leadership consists of three interrelated components: 123
- PHC policies: the decisions and plans created by governments to achieve specific PHC goals
- PHC leadership: the stewardship of those decisions and plans by governments and other stakeholders (planners, providers, patients, and communities)
- Quality management: the planning, control activities, and improvement work used to ensure high-quality PHC in practice
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Before taking action, countries should first determine whether policy & leadership is an appropriate area of focus and where to target improvement efforts. Read on to learn how to use country data to:
- Make informed decisions about where to spend time and resources
- Track progress and communicate these updates to constituents or funders
- Gain new insights into long-standing trends or surprising gaps
Countries can measure their performance using the Vital Signs Profile (VSP). The VSP is a first-of-its-kind tool that helps stakeholders quickly diagnose the main strengths and weaknesses of primary health care in their country in a rigorous, standardized way. The second-generation Vital Signs Profile measures the essential elements of PHC across three main pillars: Capacity, Performance, and Impact. Policy & leadership is measured in the Governance domain of the VSP (Capacity Pillar).
If a country does not have a VSP, it can begin to focus improvement efforts using the subsections below, which address:
- Key indications
-
If your country does not have a VSP, the indications below may help you to start to identify whether policy & leadership is a relevant area for improvement:
- Policies fall short of including fundamental elements: a defined service package, viable financing mechanism, and a monitoring & evaluation (M&E) framework.
- Current policies were established without a participatory process that engaged multiple stakeholders.
- Absence of a joint review that includes a diverse range of stakeholders assessing the progress, outcomes, strengths, and weaknesses of a policy.
- Current PHC policies are not evidence-based, lacking grounding in research-identified solutions, approaches, knowledge, experience, values, and goals.
- Current PHC policies are not embedded in a legal framework.
- There is no National Health Plan or National Strategic Plan, or PHC is not a focus of the Plan.
- There is a lack of an articulated national direction on quality, or it is focused on hospital safety and tertiary care rather than PHC.
- The PHC system does not use quality interventions to:
- Create an enabling systems environment, such as registration and licensing and performance benchmarking;
- Engage patients, such as community engagement platforms and shared decision-making tools;
- Improve clinical effectiveness, such as decision support tools and clinical protocols;
- Reduce harm, such as safety protocols and checklists.
- There are no active systems to routinely collect and publish data on quality.
- The health system lacks a shared culture of learning on quality.
- There is a lack of leadership commitment to institutionalize quality of care throughout the health system.
- Key outcomes and impact
-
Countries that improve policy & leadership may achieve the following benefits or outcomes: 45
- Improve the design of health systems to support and sustain good governance of PHC.
- Ensure evidence-based policies, strategies, and plans translate into action.
- Promote effective management and organization of services by establishing systems to coordinate, monitor, integrate, and implement policies.
- Increase service availability and quality and improve PHC functions and outcomes while minimizing harm and reducing waste.
- Make PHC functions more effective, safe, responsive, and person-centred through quality management infrastructure.
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Explore this page for a curated list of actions to improve policy & leadership, which embark on:
- An explanation of why the action is important for policy & leadership
- Descriptions of activities or interventions countries can implement to improve policy & leadership
- Descriptions of the key drivers in the health system that should be improved to maximise the success or impact of actions
- Relevant case studies, tools, or resources that showcase what other countries around the world are doing to improve policy & leadership as well as select tools and resources
Key actions:
-
Identifying and engaging key stakeholders creates a participatory process for policy development and helps create opportunities to increase accountability in the PHC system.
Key activities
National and sub-national levels
- Determine whether there is sufficient engagement and capacity within the Ministry of Health to lead or be instrumentally involved in reforms. Identify links to other government sectors and, if necessary, explore opportunities to develop them. Health in all policies “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” ( HiAP “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” ) approaches require engagement of relevant actors within and beyond the health sector as well as the promotion of actions that take health implications into consideration at every level of government. Structures like interdepartmental committees can support policy implementation and the development of broader networks for policy planning and development. At the same time, developing capacity in other ministries helps stakeholders across sectors understand the contribution of health to their own work. 6
- Identify an authority responsible for implementing the policy, knowing if it is working, and taking action to improve upon it. Identify key stakeholders by name or role, ensure that people understand their responsibilities, and educate all stakeholders on a shared understanding and definition of quality. Include operational planning and detailed implementation planning in the policy planning process to avoid challenges stemming from policies that conflict with practical realities.
- Assess the appetite for policy reform in the government and among stakeholders within the country context. Stakeholder engagement supports policy development by fostering dialogue and discussion, which can create a more welcoming environment for legitimizing and implementing policy. 7 Advocacy tools play an important role in developing and sustaining political will. Cohesion in the policy community, identification of individuals who will champion policy change, and advocacy for clear policy proposals have proven to be important steps to create an environment that supports reform. 8
- Ensure mechanisms for a participatory process and legal framework are built into the policy reform process. Health and health equity are values in their own right and policy reform processes should reflect principles of legitimacy, transparency, accountability, access to information, and collaboration in order to respect these values. 6
- Define the specific responsibilities of each important group or role. Considerations should include identifying the organizations currently active in promoting Quality improvement the action of every person working to implement iterative, measurable changes, to make health services more effective, safe, and people-centred. and how they relate to the Ministry of Health, determining the need for a task force or committee (with appropriate representatives for all stakeholders) to establish a national program, and establishing who should coordinate quality improvement at a facility level. 9
- Generate political will and sustained support, including connecting national plans to global agendas. Continuous political engagement with PHC is critical to developing sustainable and supported PHC policies, but such engagement can be hampered by inadequate advocacy, insufficient data, or a lack of focus on quality of care among other factors. In response, planners and implementers have used data (including dashboards and infographics) for lobbying; prioritized quality in national health strategies to help streamline political support; used global statements, resolutions, and commitments to garner national and local political will; and encouraged benchmarking and peer-to-peer accountability within regions to facilitate competition for improved quality. 7810
- Successful policy reform involves advocacy from political leaders who think an issue is worthy of sustained attention. 8 Use of data to illustrate the need for reform and finding the right people to help drive policy change can help establish a policy environment more receptive to change.
District and facility levels
- Ensure stakeholders are prepared for long-term investment in improving culture and behaviour necessary for successful change management. Successful adoption of quality improvement mechanisms requires that individuals and organizations change behaviours. 11 The process of managing that behaviour change is ongoing and requires multiple steps and strategies, including assessing readiness for change, ensuring environmental support (such as additional financial and human resources), developing and implementing pilot tests and plans, and anchoring change within an organization. 111213 At the point of care, health care teams should begin with simple changes in order to build success, improve morale, and create momentum to undertake more complex interventions. 13 Adopting change management practices and focusing on the individuals and groups involved can increase the likelihood that change will be successful: people, in organizations, are the ones who do, or do not, make change happen. 11
Community and civil society level
- Consider the following questions about civil society engagement. Are there mechanisms for engagement with civil society stakeholders? Is there demand for reform or policy development from this community? If not, what are the opportunities to strengthen awareness and involvement with these stakeholders?
- Ensure communities, patient organizations, and community- and faith-based organizations are represented within health system governance structures. Differences in culture and attitudes among populations are critical considerations that should be built into the processes of training and of management of local health care facilities. While national plans often mention this fact, rarely do those plans identify where funding will come from and who will be responsible for ensuring these elements are considered. Similarly, various organizations must have opportunities to collaborate on quality activities, policies, and culture. Considerations of equity and inclusion must be factored into clinical decision-making, budgeting, financial systems, and the development of human and other resources. 9
- Create opportunities and mechanisms for engagement with civil-society stakeholders in order to ensure coordination between decision-makers and other stakeholders, and hold governments and service providers accountable to communities’ needs and priorities. Civil-society engagement is a vital element of growing and sustaining a culture of quality. Patients, communities, and the media must have access to information and resources to shape their preferences and to hold providers accountable by demanding higher quality services. 121415 Community engagement Community engagement is the inclusion of local health system users and community members in all aspects of health planning, provision, and governance. It is a central component of ensuring that the services delivered are tailored to population needs, priorities and values, which can be achieved through the involvement of communities in the design, financing, governance, and implementation of PHC. To ensure that the needs of all community members are met, it is important that community engagement efforts include representation from diverse members of the community. This may require multiple mediums for engagement, to best capture the needs and opinions of traditionally underrepresented community members. can be time-intensive, and the feedback received can be challenging to integrate. Still, participation is critical and should be planned for and accommodated. 7 More information can be found in the multi-sectoral approach module.
Related elements
Relevant tools & resources
- OECD, 2021: Module on evidence-based policy making and stakeholder engagement
- WHO, 2021: Voice, agency, empowerment - handbook on social participation for universal health coverage
- WHO, 2018: Multisectoral and intersectoral action for improved health and well-being for all: mapping of the WHO European Region. Governance for a sustainable future: improving health and well-being for all: final report
- WHO, 2017: WHO community engagement framework for quality, people-centred and resilient health services
- WHO, 2016: Intersectoral planning for health and health equity
- WHO, 2012: Intersectoral governance for Health in All Policies: structures, actions and experiences
-
Accountability mechanisms help ensure policies, strategies, and plans are evidence-based and translated into action and help ensure care planning and delivery are responsive to user needs and preferences while minimizing harm and reducing waste. Monitoring, enabled by regular access to reliable data, is an important element in facilitating accountability. In addition, accountability also requires managing the balance of incentives and penalties within the system.
Key activities
National and sub-national levels
- Identify any accountability mechanisms in place to ensure a transparent, equitable, and participatory policy-making process and, if none exist currently, establish them. Approaches include peer monitoring, in which neighbouring decision-makers or stakeholders with relevant experience in policy making share their knowledge and skills while monitoring the process. Another approach is to make sure that broad stakeholder participation is part of the process from the planning stage.
- Ensure decision-makers have consistent, ongoing access to quality data. Quality data is an important element in legitimizing policy; however, many governments still struggle to integrate the use of data into policy decision-making and accountability mechanisms. Measuring quality, determining which data to use, and connecting that data to the appropriate users are crucial. Some potential approaches to strengthening data quality and access by decision-makers include data training for people at every level, development of special teams to focus on collecting and validating data, simplification of data to be collected, and support for collecting and tracking data in real-time. 7
- Ensure clear accountability for quality at all levels of service delivery, and provide the resources necessary for accountability and feedback systems to be used. Various systems and mechanisms help to reinforce quality at different levels of the health system, including M&E and supportive supervision. 9
- Monitor policy to understand its impact on health and equity of outcomes. Health impact assessments are an important component in the development of HiAP “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” policies, and governments have increasing experience with assessing the policies most likely to impact health. However, assessment cannot stop with policy development; once policies are in place, governments should continue monitoring and oversight to ensure the expected outcomes are achieved. 1214
Related elements
Relevant tools & resources
- Health Systems Strengthening Accelerator, 2020. Improving Linkages between Social Accountability and Social and Behavior Change: A Preliminary Report of Country Data Collection for Côte d’Ivoire, Ghana, and Guinea.
- UHC 2030. Toolkit on health budget literacy, advocacy and accountability for UHC.
- Health Data Governance Principles.
-
Strengthening the policy development process can improve the systems that support and sustain good governance and leadership in PHC.
Key activities
National and sub-national levels
- Ground PHC policy in data and facility-based evidence, partner with PHC stakeholders, and establish a feedback process to make sure data inform improvement. Effective national health strategy relies on data to inform the selection of priorities, clarify governance and structures, develop interventions, define a service package, and craft a practical framework for M&E. 716
- Ensure PHC policies include fundamental elements: defining a service package, identifying financing mechanisms for PHC, and establishing a system for M&E. 17
-
Use legislation, funding, and policy implementation to address health inequity. Establish a learning approach to implementation and M&E. 618
- Develop legislation and funding for policies, including the ;
- Establish clear health equity goals to guide implementation and enable equity-based evaluation; and
- Monitor and evaluate the experiences of implementation and use those lessons to inform future iterations of policy and programming.
- Encourage policymaker accountability for globally defined goals such as Sustainable Development Goals and
HiAP
“An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.”
. PHC is an important component of improving population health.
HiAP
“An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.”
approaches can complement or integrate with PHC and universal health coverage and are valuable for shedding light on health inequities and advocating for policies to address social determinants of health. Steps to implement
HiAP
“An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.”
include: 6
- Establish priorities for HiAP “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” through strategic planning and prioritization; assessment of health, equity, and health-systems-related implications; assessing policy and political contexts; and understanding governance capacities.
- Identify the context for and feasibility of implementing HiAP “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” ; data management needs; structures and processes required to support HiAP “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” implementation; and human resources, funding, and accountability implications.
- Identify supportive structures and processes, including multisectoral coordination.
- Facilitate stakeholder assessment and engagement.
- Ensure monitoring, evaluation, and reporting of progress, and disseminate lessons learned to other decision-makers to support future policy and strategy work.
- Build capacity through training or supporting health professionals in skill acquisition; building institutional and research capacity; strengthening teaching and research collaboration across sectors; building capacity across ministries; and building and supporting community capacity to participate in HiAP “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” process.
- Establish or strengthen right-to-health legislation to ensure access to health care through legal frameworks, particularly the right to PHC access. 1920
Related elements
- Multi-sectoral approach
- Adjustment to population health needs
- Information & technology
- Population health management
Relevant tools & resources
- Civil Society Engagement Mechanism for UHC2030, 2021. Health for All Advocacy Toolkit.
- Primary Health Care Performance Initiative, 2021. If Health Systems Could Talk: Illuminating the Vital Signs of Strong Primary Health Care.
- Spotlight on Sustainable Development 2021. Time for transformative policies at all levels.
- WHO 2021. Mental Health ATLAS 2020.
- 3-D Commission, 2021. Data, social determinants, and better decision-making for health.
-
Anchoring PHC policy development and reform processes in PHC institutional structures help to orient the PHC system toward supporting and sustaining good governance and leadership and toward a goal of universal health coverage.
Key activities
National and sub-national levels
- Make PHC a priority of the National Strategic Plan and ensure the PHC quality policy is linked to the strategic vision of the National Health Plan. 71018 Making PHC a priority does not require a standalone policy; countries can design their health strategies around a core of PHC by widely incorporating its five key functions: first point of contact, continuity, comprehensiveness, coordination, and patient-centred care. 21 Health policies and strategies should integrate PHC with other service delivery structures and other policy aims and emphasize the individual and community at the centre of policy and implementation. 17
- National health plan
- A National Health Plan is a dynamic, medium-term, national strategic plan that projects 3-7 years into the future and guides overall strategic reforms in a country. 1822
- Operation planning
- Operational planning can be used to develop a detailed framework for action based on strategic vision, defining key tasks, assigning responsibilities, identifying milestones, and considering practical aspects of implementation. 1618
- National strategic plan
- A National Strategic Plan links with operational planning to provide the roadmap for how the health plan will be carried out. 162324
- National health policy
-
National health policy should include explicit statements regarding 9
-
Necessary framework for policies, laws, and regulations concerning quality;
-
Equity, affordability, sustainability, and efficiency;
-
Factors (medical, technical, or organizational) that influence the quality of care;
-
Active involvement of consumers in developing indicators and standards for quality assurance in health care;
-
Appropriate incentives for participation in quality improvement;
-
Requirement of quality improvement systems as a condition for funding contracts with practitioners, hospitals, and health care organizations.
-
-
- National health plan
- Establish PHC governance structures, including a national body to coordinate, monitor, integrate, and implement national PHC policy and policy frameworks. Seek to enable a balance of local autonomy and central direction in decision-making. 24 For example, governing bodies could offer membership and decision-making authority to district- and local- level actors. Further, it is important to ensure the national coordinating body has adequate authority, budget, and staff to successfully conduct its mandate. 17
- Define clear roles and responsibilities within policies for key individuals and organizations charged with overseeing specific elements of strategy implementation. 16 Build in joint review of the progress towards PHC-related objectives with a broad range of stakeholders 17 to help ensure individuals and groups are utilized to full capacity and to help identify where responsibilities can be shared. 16 The joint review process should include assessments of context and programming; process, costs, and financing; implementation and management arrangements; and results, monitoring, and review mechanisms. With inclusive participation, this process can help improve the quality of and confidence in strategies and improve coordination. 17
- Explore mechanisms and structures to encourage collaboration across sectors to address health issues or determinants of health. For example, establish drunk driving and tobacco use laws, action plans to increase physical activity, and a national “good living plan.” 6
District level
- Create a culture of shared accountability by engaging service providers and the population in the decision-making process. Good policy engages a very broad group of stakeholders, including the workforce, district-level managers, and others who will have to operate under it. There are a variety of mechanisms that governments can implement to engage communities and civil society in national policy- and decision-making processes, including participatory governance. 2526 For additional guidance, see the WHO’s handbook on social participation for UHC.
- Create demand among users for high-quality PHC as a public right in the face of changes in political leadership. Educating and engaging communities to understand high-quality care as a right and supporting facilities in asking for resources they need to provide that quality care can help ensure that quality care is a sustained priority at the national level. 19 See action 1, sub-action 3 (engage and empower patients, families, and communities) in the service quality module for more on mechanisms.
Related elements
Multi-Sectoral Approach module
- UHC 2030. State of commitment to universal health coverage around the world.
- Cambridge University Press, 2021. Systems Thinking Analyses for Health Policy and Systems Development: A Malaysian Case Study.
- R4D, 2021. Integrating Early Detection and Treatment of Child Wasting into Routine Primary Health Care Services: A Resource Guide to Support National Planning.
- UHC 2030, 2021. Action on health systems, for universal health coverage and health security.
- Make PHC a priority of the National Strategic Plan and ensure the PHC quality policy is linked to the strategic vision of the National Health Plan. 71018 Making PHC a priority does not require a standalone policy; countries can design their health strategies around a core of PHC by widely incorporating its five key functions: first point of contact, continuity, comprehensiveness, coordination, and patient-centred care. 21 Health policies and strategies should integrate PHC with other service delivery structures and other policy aims and emphasize the individual and community at the centre of policy and implementation. 17
-
Strong quality management infrastructure supports the delivery of safe, effective, and efficient care; minimizes harm and reduces waste; and creates an environment for continuous improvement. 21427 It involves three interlinked concepts: quality planning, quality control, and quality improvement. 129
-
Quality planning Includes aims, processes, and goals needed to create an environment for continuous improvement. includes aims, processes, and goals needed to create an environment for continuous improvement.
-
Quality control Entails monitoring established processes to ensure their functionality. entails monitoring established processes to ensure their functionality.
-
Quality improvement the action of every person working to implement iterative, measurable changes, to make health services more effective, safe, and people-centred. is the action of every person working to implement iterative, measurable changes, to make health services more effective, safe, and people-centred
Key activities
National and sub-national levels
- Reaffirm leaders’ commitment to quality, such via a political declaration on quality of care 15
- Formalize these commitments via statutes, regulations, and policy and financing mechanisms. To aid in this step: 79162829
- Develop a national quality policy and strategy, and ensure that it is integrated into the formal health sector national policies, programs, and strategies. 791618
- National quality documents that should be considered:
- Develop a quality policy document as a stand-alone national document, using a multi-stakeholder process led or supported by the Ministry of Health. 16 Ensure policy review is incorporated as an element of the policy document development process.
- Develop a national quality implementation strategy, creating intercountry, national, and regional partnerships with a detailed action agenda. 791618 Ensure policy review is incorporated as an element of the quality implementation strategy development process.
- Elements that should be considered in developing a national quality policy and strategy: 16
- National health goals and priorities
- Local definition of quality
- Stakeholder mapping and engagement
- Situational analysis
- Governance and organizational structure
- Improvement methods and interventions
- Health management information and data systems (including M&E)
- Quality indicators and core measures
- National quality documents that should be considered:
- Develop a national quality policy and strategy, and ensure that it is integrated into the formal health sector national policies, programs, and strategies. 791618
- Prioritize interventions likely to have a high impact on service quality, including 3
- Interventions that reduce harm include inspections of institutions for minimum safety standards, safety protocols and checklists, and adverse event reporting.
- Interventions that improve clinical effectiveness include clinical decision support tools; clinical standards, pathways, and protocols; morbidity and mortality reviews; and collaborative and team-based improvement cycles.
- Interventions that create an enabling systems environment include registration and licensing, external accreditation, clinical governance, and public reporting.
- Interventions that engage patients, families, and communities include formalizing and empowerment mechanisms, health literacy, shared decision making, peer support and expert patient groups, patient experience of care, and patient self-management tools. 17 30
- Take advantage of a legislative environment prepared to support comprehensive PHC policies. Opportunities may occur to work in tandem or build from existing policies or policies in development, which takes advantage of momentum and lessons already learned. Policy considerations for national quality strategy development include who the stakeholders in quality in health care are, whether there is a need for an integrated national program, which should be consulted in developing a program, what relevant legislation already exists, the government’s role in creating a program, and whether mechanisms should exist to integrate external support for quality, such as from WHO or the World Bank. 9
- Create and sustain a body to plan, oversee, and steward the institutionalization of the quality management infrastructure (i.e. a national agency for quality monitoring and improvement). This group should include people representing all stakeholders affected by PHC quality structures (planners, practitioners, consumers) as well as a designated leader with clear accountability. 31
- Focus on strengthening processes that are characteristic of a well-established quality program, including information collection and sharing, a formal, sustainable policy process including all stakeholders, and independent accountability mechanisms (i.e. community engagement and public reporting mechanisms, peer reviews, accreditation, etc.) 9
- Establish and maintain health information and data systems. Use the data generated from these systems to conduct external assessments (i.e. peer review, external accreditation) and continuously improve the quality of care. 7915
- Ensure adequate financial and non-financial resources for quality improvement. 9 practices can be resource-intensive, and it is important to consider priorities and trade-offs between areas of focus as well as plan for resistance or challenges. A culture of learning must be nurtured across the health system, including at the facility, sub-national, and national levels. 15 Some critical resource considerations include: 9
- Time: Providers will spend time in training, records departments, and discussing standards, measurements, and action plans, which is time they can not spend in clinics.
- Data, information, and guidance: Clinical and management staff need access to standards, practical guidance on tested quality improvement methods, and examples of results; this guidance must be gathered and adapted for local use.
- Funding: Direct costs of quality improvement programs include quality support staff, training, data collection and access to information.
- Intentionally working across different health sector institutions and stakeholders outside the government such as health professional associations has the potential to achieve buy-in as well as gain additional resources for developing and implementing statutes, regulations and policy and financing mechanisms. 7
District and facility level
- Coordinate quality systems with national and/or local government to ensure valid standards, reliable assessments, consumer involvement, demonstrable improvement, transparency, and public access to quality criteria, procedures, and results. 9
- Embrace ongoing quality management and improvement process. Timelines of implementers and governments do not always line up; the process of institutionalizing quality management infrastructure can take as long as five to eight years, though the people involved might change more quickly. Strong leadership, effective management of staff, and a commitment to learning will aid in this transition. 9
- Establish sustainability mechanisms, and regularly revisit key steps and opportunities for users and implementers to improve processes. The appendix of the WHO report, Quality and accreditation in : a global review, 9 contains extensive learnings and recommendations about sustainable quality management, including promoting buy-in, improving training activities, and better linking different countries and agencies. Countries should pay careful attention to the feasibility of quality processes and adapt those processes for their country’s context.
- Embed quality safeguards within existing processes and programmes. Examples include:
- Encourage/promote the use of clinical decision support tools in patient care
- Ensure adherence to quality and safety protocols and standards via supportive supervision and performance measurement and management
Community and civil society level
- Involve communities in the quality management process in meaningful ways. Communities are key stakeholders in quality service delivery. 232 Strategies to solicit user and community perspectives include focus groups, key informant interviews, exit interviews, user satisfaction surveys, consumer advisory boards, needs assessments, community membership on hospital quality committees, and suggestion boxes. 121415 See action 1, sub-action 3 (engage and empower patients, families, and communities) in the service quality module for more on mechanisms.
Related elements
- Multi-sectoral approach
- Adjustment to population health needs
- Funding & allocation of resources
- Information & technology
- Management of services
Relevant tools & resources
- BMJ 2022. How to embed quality improvement into medical training
- CGD, 2022: A Higher Bar or an Obstacle Course? Peer Review and Organizational Decision-Making in an International Development Bureaucracy
- WHO, 2022: Primary health care Primary health care (PHC) is “a whole-of-society approach to health that aims to maximise the level and distribution of health and well-being through three components: (a) primary care and essential public health functions as the core of integrated health services; (b) multisectoral policy and action; and (c) empowered people and communities.” measurement framework and indicators: monitoring health systems through a primary health care lens
- WHO, 2022: Compendium of resources on quality of care
- WHO, 2020: Quality health services: a planning guide
- WHO, 2020: Operational framework for primary health care - see operational lever on systems for improving quality of care (page 58)
- WHO, World Bank, and OECD, 2019: Delivering quality health services: a global imperative for universal health coverage
- WHO, 2018: Technical series on PHC - Quality in PHC
- WHO, 2018: Handbook for national quality policy and strategy: a practical approach for developing policy and strategy to improve quality of care
- WHO, 2018: Global efforts in measuring the quality of care
- Institute for Healthcare Improvement: Improvement Capability Self-Assessment Tool
- WHO, 2017: Advancing the right to health: the vital role of law
-
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Understanding and identifying the drivers of health systems performance--referred to here as “related elements”--is an integral part of improvement efforts. We define related elements as the factors in a health system that have the potential to impact, whether positive or negative, policy & leadership. Explore this section to learn about the different elements in a health system that should be improved or prioritized to maximize the success of actions described in the “take action” section.
While there are many complex factors in a health system that can impact policy & leadership, some of the major drivers are listed below. To aid in the prioritization process, we group the ‘related elements’ into:
Upstream elements
We define “upstream elements” as the factors in a health system that have the potential to make the biggest impact, whether positive or negative, on policy & leadership.
- Multi-Sectoral Approach
-
The decisions and plans undertaken by governments should ultimately meet the needs, values, and preferences of their citizens. Thus, those decisions and plans are best when they incorporate the experience and priorities of the full spectrum of stakeholders. To achieve this, governments should adopt a multisectoral approach (also referred to as a HiAP approach), which means intentionally involving and coordinating across entities whose work touches on PHC, including governments, communities, civil society, private sector, payers, provider associations, and other nongovernmental organizations.
This approach also promotes social accountability, which helps to mitigate corruption, support quality assurance and improvement, and improve the effectiveness of decisions and plans at all levels of the health system. However, social accountability mechanisms (i.e. public reporting, citizen engagement committees, etc.) must be embedded into all aspects of health care planning, policy-making, and monitoring and evaluation to realize these benefits.
- Adjustment to Population Health Needs and Information & Technology
-
Priority setting, M&E, innovation & learning, surveillance (components of adjustment to population health needs), and health information systems are mutually reinforcing mechanisms for PHC policies and agenda-setting. These systems and processes enable countries to collect and evaluate information about population health status and needs over time. Governments can, in turn, use this information to develop more accurate, evidence-based policies and plans for their people. They can also use it to identify and learn from past challenges, which is an important aspect of quality improvement.
Learn more in the adjustment to population health needs and information & technology modules.
- Funding & Allocation of Resources
-
Whether health funding or health policies come first depends on the context; however, both are mutually strengthening mechanisms. Many countries have limited resources to allocate for PHC and/or limited control over how resources are allocated. This is especially the case in aid-dependent settings, where funding flows are influenced by external donors and global health initiatives. 33 Thus, financing reforms which prioritize health systems strengthening and PHC-oriented models of care will be critical to the success of PHC policies and quality initiatives. For example, reforms should increase the financing available for PHC and reduce inefficiencies in the health system, such as the overreliance on hospitals to deliver primary care. Furthermore, increased and sustained funding for PHC would allow countries more flexibility to make PHC in the long term. 2
- Population Health Management
-
Priority setting at the local level, a component of population health management, enables the collection and use of local data. This also allows for the alignment of national and subnational policies with local priorities and agendas (and vice versa). Additionally, community engagement supports the involvement of local stakeholders in the planning of PHC policies. As individuals in leadership positions change, often more quickly than policy development and implementation processes occur, ongoing community engagement can help to guarantee sustained oversight and demand for the policies that are developed and to hold policymakers accountable for the effects of these policies over time.
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Countries seeking to improve policy & leadership can pursue a wide array of potential improvement pathways. The short case studies below highlight promising and innovative approaches that countries around the world have taken to improve.
PHCPI-authored cases were developed via an examination of the existing literature. Some also feature key learnings from in-country experts.
- East Asia & the Pacific
- Europe & Central Asia
- Latin America & the Caribbean
- Middle East & North Africa
- North America
- South Asia
- Sub-Saharan Africa
-
- Ethiopia: Using regulatory mechanisms to improve the quality and resilience of services
- Ethiopia: Strengthening Primary Health Care Systems to Increase Effective Coverage and Improve Outcomes in Ethiopia
- Kenya: Embedding quality improvement at all levels of the health system
- Malawi: Evidence-Based Reproductive Health Policy Development for Young People
- South Africa: Integrating health technology assessment and the right to health: a qualitative content analysis of procedural values in South African judicial decisions
- Multiple regions
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Policy & leadership is a crucial part of PHC governance. According to the WHO building blocks of a health system, governance includes “ensuring strategic policy frameworks exist and are combined with effective oversight, coalition-building, regulation, attention to system design, and accountability.” 34 Strong, effective governance underpins all the functions and processes of a successful PHC system. Policy & leadership represent both the plan for a high-functioning PHC system and the will to enact that plan.
Below, we define some of the characteristics of policy & leadership in greater detail:
-
PHC leadership refers to the level of political commitment and leadership to PHC. PHC leadership begins with a national authority (or authorities) for PHC within the government responsible for providing stewardship of PHC. This person or governmental entity must have accountability for the entire range of comprehensive PHC services PHC services refer to any intervention, procedure, regimen, or process that providers use to respond to the needs and demands of their patient population at the primary care level. Because of PHC’s community-facing orientation, services can be provided virtually or face-to-face in homes, communities, or PHC centres. Depending on the context, services may be provided by public or private providers. as defined by national health policies, strategies, and/or plans. The mandate of this authority should include the public sector as well as oversight and regulation of the private sector, where applicable, and must include oversight of all functions relevant to PHC to ensure active alignment and coordination for the effective and efficient delivery of PHC services PHC services refer to any intervention, procedure, regimen, or process that providers use to respond to the needs and demands of their patient population at the primary care level. Because of PHC’s community-facing orientation, services can be provided virtually or face-to-face in homes, communities, or PHC centres. Depending on the context, services may be provided by public or private providers. . 15
Strong PHC leadership is marked by: 7916282935
- Formalized commitments to PHC: Leadership invests in PHC, places it at the centre of efforts to achieve universal health coverage and the SDGs, and raises awareness about its importance across the health system. Leadership may use declarations, laws, policies, and financing mechanisms to formalize commitments to PHC, among others.
- Coordinated, multisectoral policy and action: Leadership implement a approach to ensure that PHC is treated as a priority within and beyond the health sector and that resultant plans align with diverse stakeholder interests. Furthermore, they coordinate, monitor, integrate, and implement national policies related to PHC with defined authority, clear accountability, adequate budget, and sufficiently competent staff.
- Enabling legal environment for PHC: Governments realize commitments to PHC and its citizens via health laws and legal practices such as .
-
PHC policies are a deliberate system of guidelines or plans that countries adopt in support of PHC. They serve as the basis for making decisions and help a country to improve and develop the functions it needs to achieve desired goals. The main functions of PHC-oriented health systems are financing, stewardship, resource development, and the provision of health services that place PHC as the first point of contact. 12
Making PHC a priority does not require a standalone policy. Policies designed around PHC put PHC at the core of a country’s health strategy. They emphasize the five key functions of primary health care: first point of contact, continuity, comprehensiveness, coordination, and patient-centred care. 21 They integrate primary care with other service delivery structures and other policy aims and objectives and emphasize the individual and community at the centre of policy and implementation. 17 To promote a PHC-oriented health system, PHC should be emphasized in the following policies, strategies, or plans:
- A National Health Plan (national policy document) is a dynamic medium-term national strategic plan that looks 3-7 years into the future and guides overall strategic reforms in a country 1822
- A National Strategic Plan (national policy document) links with operational planning to provide the roadmap (national policy document) for how the health plan will be carried out. 1624
Furthermore, to promote PHC-oriented models of care, the national health policy should include the following themes and/or areas of work: 1236
- Existence of a national health sector policy-oriented to PHC and UHC
- Existence of a national policy, strategy, or plan on quality and patient safety
- Existence of health emergency and disaster risk management strategies
- Institutional capacity to meet essential public health functions and operations
And the policy(s) should be developed and implemented via the following principles and processes:
- : Policy makers use data and facility-based evidence to inform the selection of priorities, clarify governance and structures, develop interventions and define a service package, and craft a practical framework for monitoring and evaluation. 1637
- Multisectoral action and community leadership: Policy makers ensure a unified vision and priority for high-quality PHC as a public right in the face of changes in political leadership. They help to sustain PHC as a priority by educating and engaging communities to understand high-quality care as a right and working with facilities to ask for the support and resources they need to provide that quality care. 7 PHC policies also depend on strong governmental leadership because leaders are responsible for establishing, promoting, and implementing PHC policies. 38
- Transparency and mutual accountability: Policies are developed via a transparent, participatory process and policymakers are held accountable for the impacts of these policies at all levels. Diverse stakeholders --- including the private sector, civil society, and communities --- are given a legitimate, equal voice in this process. 2638
- Integrated, people-centred approach: Policies are developed via a HiAP “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” approach and designed and developed according to the local context, values, and preferences. Policies promote integrated, people-centred health services (i.e. calling for multidisciplinary teams, prioritizing community- and family-oriented models of care, etc.). 232
-
Quality management infrastructure includes the planning, control activities, and improvement work that ensure populations receive high-quality health services while minimizing harm and resource waste. 9 Strong quality management infrastructure supports the delivery of safe, effective, and efficient care; minimizes harm and reduces waste; and creates an environment for continuous improvement. Such infrastructure must be built upon and integrated into appropriate PHC policies and leadership and, as a continuous process, is reliant on sustainability planning built into strong PHC policies.
The predominant functions of governing quality of care at the national and subnational levels encompass leadership and management; the establishment of laws and policies; regulation; monitoring and evaluation; planning; and financing mechanisms. 7 A well-considered national quality strategy and operational plan are critical to institutionalizing quality management. It is important that quality management structures are developed with buy-in from stakeholders at every level: fostering a “culture of quality” is as important to the success of quality infrastructures as having a plan in place. Quality cannot be “inspected into” PHC systems if clinical staff are not committed participants; national mandates for need supporters and champions. At the same time, that culture alone is not sufficient to guarantee safety, efficiency, and accountability. 9
Identification and implementation of appropriate quality interventions can have a significant impact on the delivery of specific health services and on the health system at large. Most approaches to national quality strategy development involve one or more of the following processes:
- A quality policy and implementation strategy as part of the formal health sector national plan;
- A quality policy document developed as a stand-alone national document is usually developed from a multi-stakeholder process led or supported by the ministry of health;
- A national quality implementation strategy with a detailed action agenda, which also includes a section on essential policy areas;
- Enabling legislation and regulatory statutes to support the policy and strategy.
-
Designing and supporting effective PHC policies ensures a strong foundation for a successful PHC system. Fortunately, a great deal is known about how to improve health outcomes, and many technological tools are available to further these efforts. Increasingly, the challenge for PHC systems is not to determine what must be done to improve population health but instead to garner the political will and unite states and stakeholders to prioritize health and health care goals. 35
Below, we summarize common frameworks and approaches that countries can use to strengthen policy & leadership for PHC in their context.
Right to Health
National health policies should seek to strengthen PHC in order to increase equitable access to health care and should be underpinned by . 26 The human right to health is enshrined in many global governance documents; however, in practice, gaps remain in equitable access to health care. The Sustainable Development Goals emphasize countries’ commitment to universal health coverage,(7) and an important pathway to achieving universal health coverage is by strengthening PHC systems. 89 10
What is included in the Right to Health?
The bullets below are adapted from WHO Office of the United Nations High Commissioner for Human Rights Factsheet 31: The Right to Health.
- The right to underlying determinants of health, including:
- Safe drinking water and adequate sanitation
- Safe food
- Adequate nutrition and housing
- Healthy working and environmental conditions
- Health-related education and information
- Gender equality
- The right to freedoms from:
- Non-consensual medical treatment, such as medical experiments and research or forced sterilization
- Torture and other cruel, inhuman, or degrading treatment or punishment
- The right to entitlements:
- The right to a system of health protection provides equality of opportunity for everyone to enjoy the highest attainable level of health
- The right to prevention, treatment, and control of diseases
- Access to essential medicines
- Maternal, child, and reproductive health
- Equal and timely access to basic health services
- The provision of health-related education and information
- Participation of the population in health-related decision-making at the national and community levels
- Health services, goods, and facilities must be provided to all without discrimination.
- Services, goods, and facilities must be available, accessible, acceptable, and of good quality.
- Functioning public health and health-care facilities, goods, and services must
- Be available in sufficient quantity.
- Be accessible physically (in safe reach for all sections of the population, including children, adolescents, older persons, persons with disabilities, and other vulnerable groups) as well as financially and on the basis of non-discrimination.
- Respect medical ethics and be gender-sensitive and culturally appropriate.
- Be scientifically and medically appropriate and of good quality. This requires trained health professionals, scientifically approved and unexpired drugs and hospital equipment, adequate sanitation, and safe drinking water.
Health in All Policies
builds upon the approach by encouraging strong PHC policies through understanding and addressing the multisectoral nature of health. HiAP “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” understands, first, that good health is essential for a strong economy and for a population to thrive. Second, HiAP “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” acknowledges that social determinants of health are essential contributors to health outcomes but that such determinants are shaped primarily by decisions made outside of the health sector. WHO’s HiAP “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” framework for country action calls on ministries of health to engage with other sectors of government “through leadership, partnership, advocacy, and mediation” in order to achieve health outcomes. Multisectoral coordination is, therefore, an essential element for successful HiAP “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” approaches. 26
- The right to underlying determinants of health, including:
-
- Community engagement Community engagement is the inclusion of local health system users and community members in all aspects of health planning, provision, and governance. It is a central component of ensuring that the services delivered are tailored to population needs, priorities and values, which can be achieved through the involvement of communities in the design, financing, governance, and implementation of PHC. To ensure that the needs of all community members are met, it is important that community engagement efforts include representation from diverse members of the community. This may require multiple mediums for engagement, to best capture the needs and opinions of traditionally underrepresented community members. : Community engagement Community engagement is the inclusion of local health system users and community members in all aspects of health planning, provision, and governance. It is a central component of ensuring that the services delivered are tailored to population needs, priorities and values, which can be achieved through the involvement of communities in the design, financing, governance, and implementation of PHC. To ensure that the needs of all community members are met, it is important that community engagement efforts include representation from diverse members of the community. This may require multiple mediums for engagement, to best capture the needs and opinions of traditionally underrepresented community members. is the inclusion of local health system users and community members in all aspects of health planning, provision, and governance. It is a central component of ensuring that the services delivered are tailored to population needs, priorities and values, which can be achieved through the involvement of communities in the design, financing, governance, and implementation of PHC. To ensure that the needs of all community members are met, it is important that community engagement efforts include representation from diverse members of the community. This may require multiple mediums for engagement, to best capture the needs and opinions of traditionally underrepresented community members.
- Deliberative process A deliberative dialogue or process is a “process of collective and procedural discussion where an inclusive and representative set of stakeholders consider facts from multiple perspectives, converse with one another to think critically about options, and through reasoned argument refine and enlarge their perspectives, opinions and understandings.” : A deliberative dialogue or process is a “process of collective and procedural discussion where an inclusive and representative set of stakeholders consider facts from multiple perspectives, converse with one another to think critically about options, and through reasoned argument refine and enlarge their perspectives, opinions and understandings.” 39
- Health benefits or service package “The type and scope of health services that a purchaser buys from providers on behalf of its beneficiaries.” : “The type and scope of health services that a purchaser buys from providers on behalf of its beneficiaries.” 2
- Health care services Health care services refer to any intervention, procedure, regimen, or process that health workers use to respond to the needs and demands of their patient population. Depending on the context, services may be provided by public or private providers. : Health care services Health care services refer to any intervention, procedure, regimen, or process that health workers use to respond to the needs and demands of their patient population. Depending on the context, services may be provided by public or private providers. refer to any intervention, procedure, regimen, or process that health workers use to respond to the needs and demands of their patient population. Depending on the context, services may be provided by public or private providers. 678
- Health data “In public health, “data” usually refers to statistics reported from health care facilities, survey data or data collected through observational studies. Distinctions can be made between routinely reported data and data that are collected at certain times or over a specific period of time as part of a special study or survey. Both routine and non-routine data, as well as data from research systems, are required and contribute to a fuller picture of any given public health issue.” : “In public health, “data” usually refers to statistics reported from health care facilities, survey data or data collected through observational studies. Distinctions can be made between routinely reported data and data that are collected at certain times or over a specific period of time as part of a special study or survey. Both routine and non-routine data, as well as data from research systems, are required and contribute to a fuller picture of any given public health issue.” 40
- Health governance “The wide range of steering and rule-making related functions carried out by governments and decision-makers as they seek to achieve national health policy objectives. Governance is a political process that balances competing influences and demands. It includes: maintaining the strategic direction of policy development and implementation; detecting and correcting undesirable trends and distortions; articulating the case for health in national development; regulating the behaviour of a wide range of actors, from health care financiers to health care providers; and establishing transparent and effective accountability mechanisms.” : “The wide range of steering and rule-making related functions carried out by governments and decision-makers as they seek to achieve national health policy objectives. Governance is a political process that balances competing influences and demands. It includes: maintaining the strategic direction of policy development and implementation; detecting and correcting undesirable trends and distortions; articulating the case for health in national development; regulating the behaviour of a wide range of actors, from health care financiers to health care providers; and establishing transparent and effective accountability mechanisms.” 2
- Health in all policies “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” ( HiAP “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” ): “An approach to public policies across sectors that systematically takes into account the implications for health and health systems of decisions, seeks collaborations, and avoids harmful health impacts in order to improve population health and health equity. A Health in All Policies approach is founded on health-related rights and obligations. It emphasizes the effect of public policies on health determinants and aims to improve the accountability of policy-makers for the effects on health of all levels of policymaking.” 2
- Information systems for health “A health information system (HIS) is broadly defined as a system that integrates data collection, processing, reporting, and use of the information necessary for improving health service effectiveness and efficiency through better management at all levels of health services. It encompasses all health data sources including health facility and community data; electronic health records for patient care; population-based data; human resources information; financial information; supply chain information; and surveillance information, along with the use and communication of this information.” : “A health information system (HIS) is broadly defined as a system that integrates data collection, processing, reporting, and use of the information necessary for improving health service effectiveness and efficiency through better management at all levels of health services. It encompasses all health data sources including health facility and community data; electronic health records for patient care; population-based data; human resources information; financial information; supply chain information; and surveillance information, along with the use and communication of this information.” 41
- M&E platform: “M&E platform” is used to describe various mechanisms used to support national and subnational monitoring, evaluation, and review efforts. The primary aim of the platform is to better align and reduce duplication of these efforts among key partners (i.e. governments, donors, and development organizations, among others). To simplify, we will use the M&E system and M&E platform interchangeably in this module.
- Quality improvement the action of every person working to implement iterative, measurable changes, to make health services more effective, safe, and people-centred. is the action of every person working to implement iterative, measurable changes, to make health services more effective, safe, and people-centred.
- Quality control Entails monitoring established processes to ensure their functionality. entails monitoring established processes to ensure their functionality.
- Quality planning Includes aims, processes, and goals needed to create an environment for continuous improvement. includes aims, processes, and goals needed to create an environment for continuous improvement.
- Right to health legislation “The right to the highest attainable standard of health” implies a clear set of legal obligations on states to ensure appropriate conditions for the enjoyment of health for all people without discrimination…The right to health is one of a set of internationally agreed human rights standards and is inseparable or ‘indivisible’ from these other rights. This means achieving the right to health is both central to, and dependent upon, the realisation of other human rights, to food, housing, work, education, information, and participation.” : “The right to the highest attainable standard of health” implies a clear set of legal obligations on states to ensure appropriate conditions for the enjoyment of health for all people without discrimination…The right to health is one of a set of internationally agreed human rights standards and is inseparable or ‘indivisible’ from these other rights. This means achieving the right to health is both central to, and dependent upon, the realisation of other human rights, to food, housing, work, education, information, and participation.” 20
- Social accountability A measure of whether a country is held accountable to existing and emerging social concerns and priorities based on needs relevant to PHC of internal and external stakeholders. is a measure of whether a country is held accountable to existing and emerging social concerns and priorities based on need relevant to PHC of internal and external stakeholders.
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
References:
- WHO. Primary health care measurement framework and indicators: monitoring health systems through a primary health care lens [Internet]. World Health Organization. 2022 [cited 2022 Mar 1]. Available from: https://www.who.int/publications/i/item/9789240044210
- WHO. Primary Health Care Transforming Vision into Action: Operational Framework. World Health Organization; 2018.
- WHO, OECD, The World Bank. Delivering quality health services: A global imperative for universal health coverage. Geneva: WHO, The World Bank, and OECD; 2018.
- WHO, UNICEF. Internal working draft: Primary health care performance: measurement for improvement- technical specifications. WHO; 2021 Oct.
- Armstrong, M. & Baron, A. (1998), Performance Management Handbook, IPM, London [Internet]. [cited 2019 Jan 30]. Available from: http://www.sciepub.com/reference/151290
- WHO. Health in All Policies (HiAP) framework for country action. Health Promot Int. 2014 Jun;29 Suppl 1:i19-28.
- Tarantino L, Laird K, Ottosson A, Frescas R, et al. Institutional Roles and Relationships Governing the Quality of Health Care. Bethesda, MD: Health Finance & Governance Project, Abt Associates and USAID Applying Science to Strengthen and Improve Systems Project, URC; 2016 Aug.
- Shiffman J. Generating political priority for maternal mortality reduction in 5 developing countries. Am J Public Health. 2007 May;97(5):796–803.
- WHO. Quality and accreditation in health care services: a global review. 2003 [cited 2020 May 29]; Available from: https://www.who.int/hrh/documents/en/quality_accreditation.pdf
- WHO. Primary health care: transforming vision into action - Operational Framework. Global Conference on Primary Health Care. 2018;
- Varkey P, Antonio K. Change management for effective quality improvement: a primer. Am J Med Qual. 2010 Aug;25(4):268–73.
- Moulding NT, Silagy CA, Weller DP. A framework for effective management of change in clinical practice: dissemination and implementation of clinical practice guidelines. Quality and Safety in Health Care. 1999 Sep 1;8(3):177–83.
- Necochea E, Tripathi V, Kim Y-M, Akram N, Hyjazi Y, da Luz Vaz M, et al. Implementation of the Standards-Based Management and Recognition approach to quality improvement in maternal, newborn, and child health programs in low-resource countries. Int J Gynaecol Obstet. 2015 Jun;130 Suppl 2:S17-24.
- WHO. Quality health services: a planning guide. World Health Organization; 2020.
- PHCPI. Primary Health Care Progression Model Assessment Tool [Internet]. Primary Health Care Progression Model Assessment Tool. 2019. Available from: https://improvingphc.org/sites/default/files/PHC-Progression%20Model%202019-04-04_FINAL.pdf
- WHO. Handbook for national quality policy and strategy: a practical approach for developing policy and strategy to improve quality of care. Geneva: WHO; 2018.
- Primary Health Care Performance Initiative (PHCPI). Primary Health Care Progression Model Assessment Tool. 2019 [cited 2020 May 29]; Available from: https://improvingphc.org/sites/default/files/PHC-Progression%20Model%202019-04-04_FINAL.pdf
- WHO. Strategizing national health in the 21st century: a handbook [Internet]. Schmets G, Rajan D, Kadandale S, editor. Geneva: World Health Organization; 2016 [cited 2019 Dec 17]. Available from: https://apps.who.int/iris/handle/10665/250221
- Ranabhat CL, Kim C-B, Singh A, Acharya D, Pathak K, Sharma B, et al. Challenges and opportunities towards the road of universal health coverage (UHC) in Nepal: a systematic review. Arch Public Health. 2019 Feb 4;77:5.
- WHO. Human rights and health [Internet]. WHO. 2017 [cited 2022 May 19]. Available from: https://www.who.int/news-room/fact-sheets/detail/human-rights-and-health
- Bitton A, Veillard JH, Basu L, Ratcliffe HL, Schwarz D, Hirschhorn LR. The 5S-5M-5C schematic: transforming primary care inputs to outcomes in low-income and middle-income countries. BMJ Glob Health. 2018 Oct 2;3(Suppl 3):e001020.
- Ministry of Health Viet Nam. Plan for people’s health protection, care and promotion 2016-2020. 2016;
- Ethiopian Federal Ministry of Health. Health Sector Transformation Plan (2015/16-2019/20). Ethiopian Federal Ministry of Health; 2015 p. 1–118. Report No.: May.
- Ethiopian Federal Ministry of Health. Health Sector Transformation Plan (2015/16-2019/20). Ethiopian Federal Ministry of Health; 2015 p. 1–118. Report No.: May.
- WHO. Voice, agency, empowerment - handbook on social participation for universal health coverage. WHO; 2021 May.
- Sacks E, Morrow M, Story WT, Shelley KD, Shanklin D, Rahimtoola M, et al. Beyond the building blocks: integrating community roles into health systems frameworks to achieve health for all. BMJ Glob Health. 2018;3(Suppl 3):e001384.
- Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Health. 2018 Nov;6(11):e1196–252.
- National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Health Care Services, Board on Global Health, Committee on Improving the Quality of Health Care Globally. Crossing the global quality chasm: improving health care worldwide. Washington (DC): National Academies Press (US); 2018.
- Mbindyo R, Kioko J, Siyoi F, Cheruiyot S, Wangai M, Onsongo J, et al. Legal and institutional foundations for universal health coverage, Kenya. Bull World Health Organ. 2020 Oct 1;98(10):706–18.
- WHO, World Bank, OECD. Delivering quality health services: A global imperative for universal health coverage. WHO, World Bank, and OECD; 2018.
- WHO, World Bank, OECD. Delivering quality health services: A global imperative for universal health coverage. WHO, World Bank, and OECD; 2018.
- WHO. Framework on integrated, people-centred health services. World Health Organization; 2016.
- Terwindt F. Priority-setting for national health policies, strategies and plans. Soucat A, editor. World Health Organization; 2016.
- WHO. Monitoring the Building Blocks of Health Systems: A handbook of indicators and their measurement strategies. World Health Organization; 2010.
- Kickbusch I, Szabo MMC. A new governance space for health. Glob Health Action. 2014 Feb 13;7:23507.
- Rentschler J, Klaiber C, Tariverdi M, Desjonqueres C, Mercadante J. Frontline : Preparing Healthcare Systems for Shocks from Disasters to Pandemics. World Bank, Washington, DC; 2021 Apr.
- USAID. Health Finance and Governance Project: Final Country Reports. USAID; 2015.
- Brinkerhoff DW, Bossert TJ. Health Governance: Concepts, Experience, and Programming Options. USAID; 2008.
- Canada Institute for Health Research. Deliberative Priority Setting – a CIHR KT module [Internet]. 2010 [cited 2022 Mar 20]. Available from: https://cihr-irsc.gc.ca/e/43533.html
- WHO/Europe. European health report 2018 - Chapter 4: Defining the vision for harmonized and interoperable information systems for health in Europe [Internet]. WHO/Europe. 2018 [cited 2022 Apr 26]. Available from: https://www.euro.who.int/en/data-and-evidence/european-health-report/european-health-report-2018/chapter-4
- United Nations Development Programme. Health information systems: the importance of health information systems [Internet]. 2021 [cited 2022 Apr 26]. Available from: https://www.undp-capacitydevelopment-health.org/en/capacities/focus/health-information-systems/
