|
|
|
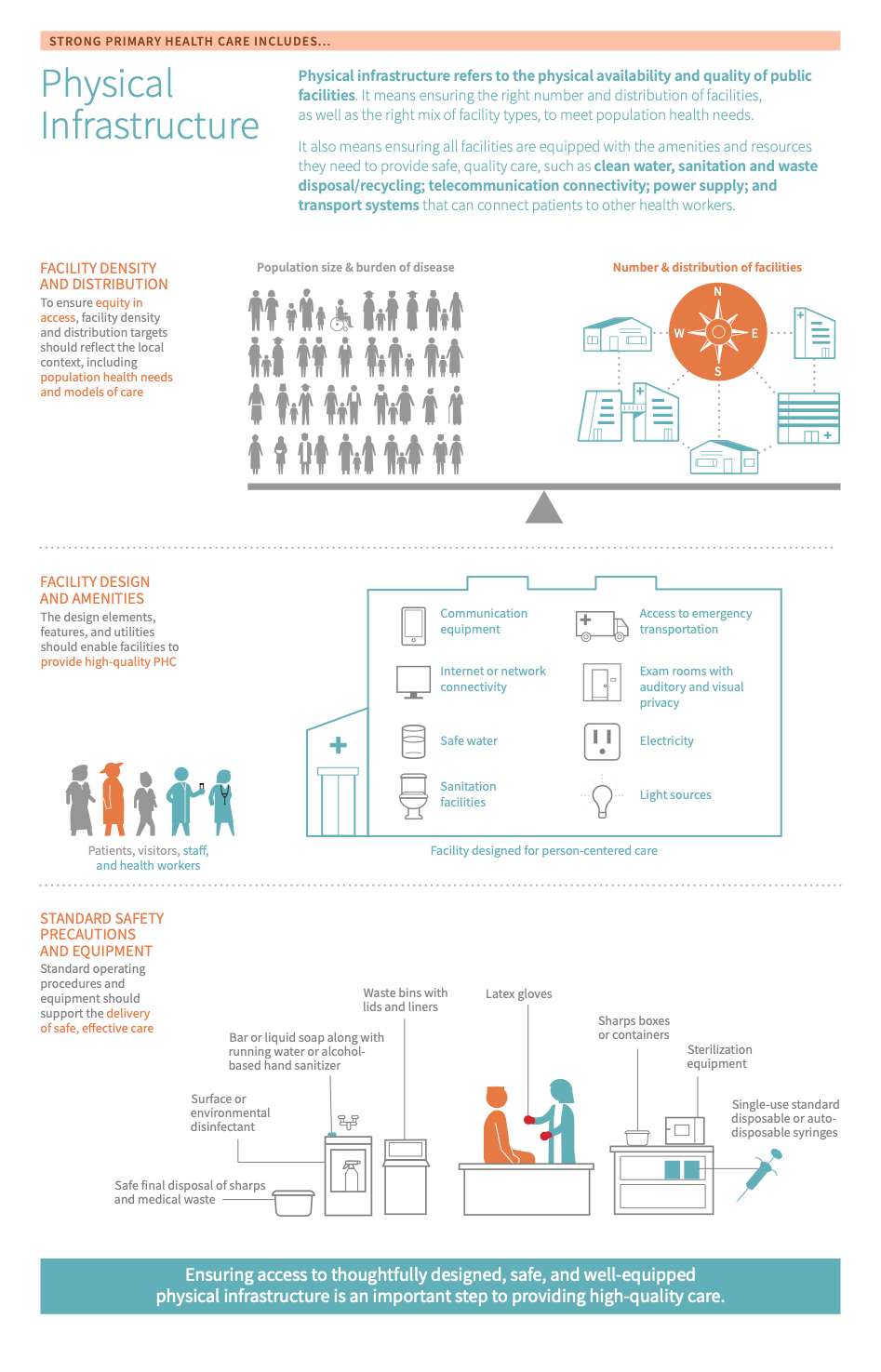
Ensuring access to thoughtfully designed, safe, and well-equipped facility infrastructure is an important step to providing high-quality PHC.
Physical infrastructure refers to the physical availability and quality of public facilities, including the number of facilities, facility amenities and resources, the distribution of facilities, and the appropriate mix of facility types to meet population health needs.
Physical infrastructure refers to the physical availability and quality of public facilities, including the number of facilities, facility amenities and resources, the distribution of facilities, and the appropriate mix of facility types to meet population health needs. Facility amenities Facility amenities are the features and utilities that enable primary care facilities to be ready and able to provide quality, person-centered primary health care. Basic amenities include electricity, safe water, exam rooms with auditory and visual privacy, light sources, sanitation facilities (toilet/latrine: flush/pour toilets to piped sewer system or septic tank, pit latrine, composting toilet), communication equipment (cell phone, landline telephone, and/or shortwave radio), computer with internet or network connectivity, and access to emergency transportation. and resources include those which are essential to the provision of safe care, including water, sanitation and waste disposal/recycling, telecommunication connectivity, power supply, as well as transport systems that can connect patients to other care providers.
In spite of their importance, gaps still remain in ensuring sufficient facility amenities, safety precautions, and equipment. An important step for prioritizing health infrastructure needs and priorities is to gather data that describe current conditions, including what health care systems and facilities are lacking in addition to what they have. A lack of appropriate facility amenities and sufficient safety precautions and equipment exposes people seeking primary health care, the facility staff, and health care providers to a greater risk of infection and disease. This can happen through contaminated water, hands, food, medical equipment, inadequate sharps and infectious waste disposal, and the potential for unsafe blood transfusions.6
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Every country should work to improve their physical infrastructure. Before taking action, countries should first determine where to target improvement efforts. Read on to learn how to use country data to:
- Make informed decisions about where to spend time and resources
- Track progress and communicate these updates to constituents or funders
- Gain new insights into long-standing trends or surprising gaps
Countries can measure their performance using the Vital Signs Profile (VSP). The VSP is a first-of-its-kind tool that helps stakeholders quickly diagnose the main strengths and weaknesses of primary health care in their country in a rigorous, standardized way. The second-generation Vital Signs Profile measures the essential elements of PHC across three main pillars: Capacity, Performance, and Impact. Physical infrastructure is measured in the Inputs domain of the VSP (Capacity Pillar).
If a country does not have a VSP, it can begin to focus improvement efforts using the subsections below, which address:
- Key indications
-
If your country does not have a VSP, the indications below may help you to start to identify whether physical infrastructure is a relevant area for improvement:
- High risk for infection and disease: if patients, providers, and facility staff are frequently at risk for infection and disease due to factors such as contaminated water, food, or medical equipment, inadequate sharps and infectious waste disposal, and potential for unsafe blood transfusion then it may indicate poor physical infrastructure.
- Infrequent facility assessments and/or data on facility conditions: if there is little to no data on current conditions and what is lacking at the facility, such as tools to measure service availability, readiness, and provision then this may indicate a need to improve assessment tools for physical infrastructure.
- Fragmented and/or poor quality WASH amenities: if the facility does not provide all four of water, sanitation, hygiene, and waste management services, this is an indication that a health facility is not performing well with regard to strong physical infrastructure.
- Frequent power outages: if the facility lacks reliable energy sources, this is an indication of poor physical infrastructure.
- Key outcomes and impact
-
Countries that work to strengthen their physical infrastructure may achieve the following benefits or outcomes:
- Improving access to care: well-designed and equitably distributed facility infrastructure helps to ensure that all populations have timely, geographic access to care and increase a health system’s ability to deliver services.
- Monitoring & continuous quality improvement: understanding essential health system performance indicators can allow for countries to utilize data that promotes action as it identifies areas for improvement surrounding physical infrastructure.
- Culture of safety: sufficient facility infrastructure, including standard safety precautions and equipment, helps to promote a culture of safety, in turn helping to improve clinical outcomes and patient experience of care.
- Improved outcomes: reducing the risk of infection and disease for patients, facility staff, and health care providers by providing appropriate facility amenities
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Explore this page for a curated list of actions to improve physical infrastructure, which embark on:
- An explanation of why the action is important for a country’s physical infrastructure
- Descriptions of activities or interventions countries can implement to improve physical infrastructure
- Descriptions of the key drivers in the health system that should be improved to maximise the success or impact of actions
- Relevant tools & resources
Key actions:
-
Ensuring there are standards set for safety, safety equipment and procedures is crucial in helping to control infection and the spread of infection within a health facility. Enforcing safety standards also works to provide a high level of protection for patients, health care workers and visitors.
Key activities
Policy Level
- Establish standards at a national level for infection prevention and control.12
- Creation and maintenance of a Master Facility List A Master Facility List is a complete listing of health facilities in a country, both public and private. It is composed of a set of administrative information and data that identifies each facility – such as facility codes, names, types, ownership or managing authority, location, address, and contact information, geographic coordinates, and operational status, as well as services offered, human resources, and infrastructure details such as number of inpatient beds – and is used as a standard mechanism for uniquely identifying health facilities and allowing for information to be compared across time and across data sources for individual facilities. .12
Operational Level
- Prioritize infection prevention and control.12
- Adhere to national standards surrounding safety equipment and procedures.
- Ensure effective maintenance and management of health facilities.12
- Facility assessment and reporting: create and utilize mechanisms for reporting on the standards set for a given health facility and how facilities are functioning, in general.12
Related elements
- Policy & leadership
- Adjustment to population health needs
- Resilient facilities & services
- Management of services
Relevant tools & resources
- The Joint Commission has developed standards for a variety of IPC topics here.
- This WHO website provides links to new guidelines on core components of IPC at the national and acute health care facility levels.
- The WHO developed this Master Facility List A Master Facility List is a complete listing of health facilities in a country, both public and private. It is composed of a set of administrative information and data that identifies each facility – such as facility codes, names, types, ownership or managing authority, location, address, and contact information, geographic coordinates, and operational status, as well as services offered, human resources, and infrastructure details such as number of inpatient beds – and is used as a standard mechanism for uniquely identifying health facilities and allowing for information to be compared across time and across data sources for individual facilities. Resource Package, which offers guidance for countries wanting to strengthen their Master Facility List A Master Facility List is a complete listing of health facilities in a country, both public and private. It is composed of a set of administrative information and data that identifies each facility – such as facility codes, names, types, ownership or managing authority, location, address, and contact information, geographic coordinates, and operational status, as well as services offered, human resources, and infrastructure details such as number of inpatient beds – and is used as a standard mechanism for uniquely identifying health facilities and allowing for information to be compared across time and across data sources for individual facilities. .
- There are a variety of health facility assessment tools designed to assess and monitor the service availability and readiness of their facilities, including:
- The Service Availability and Readiness Assessment (SARA) - WHO
- The Service Provision Assessment (SPA) - USAID
- The Harmonized Health Facility Assessment (HHFA) - WHO
- Facility assessment tool - IHI
- Patient safety assessment tool - IHI
-
Ensuring a health facility is equipped with the most basic features and utilities are essential to a strong and effective physical infrastructure. Without these basic essentials, a health facility likely cannot provide high-quality primary care to its patients.
Key activities
Policy level
- Implement strategies to ensure all health facilities have safe water and sanitation (WASH).12
- Develop plans to ensure all health facilities are connected to a reliable power supply and have effective telecommunications connectivity.12
- Create policies that work to promote physical access to health facilities for all.12
Facility level
- Reliable power supply: ensure that all health facilities are connected to a reliable power supply
- Reliable WASH system: ensure that all health facilities have reliable WASH systems.12
- Promote effective management and maintenance of health facilities, including the prioritization of telecommunications connectivity, effective water and sanitation systems, and internet connectivity.12
Community level
- Address issues related to transport to ensure patients can access services when they need it most.12
Related elements
- Policy & leadership
- Funding & allocation of resources
- Management of services
- Resilient facilities & services
- Access
- Primary care Primary care is “a key process in the health system that supports first-contact, accessible, continuous, comprehensive, and coordinated patient-focused care.” functions
Relevant tools & resources
- The USAID offers health facility guidelines and management benchmarks here
- The WHO offers a variety of tools that health managers can use to manage service delivery data here
- The WHO offers a variety of tools & materials related to WASH compliance here
- The WHO offers a compendium of resources and guidelines on safer primary care here
- USAID developed the Powering Health Toolkit
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Understanding and identifying the drivers of health systems performance--referred to here as “related elements”--is an integral part of improvement efforts. We define related elements as the factors in a health system that have the potential to impact, whether positive or negative, physical infrastructure. Explore this section to learn about the different elements in a health system that should be improved or prioritized to maximize the success of actions described in the “take action” section.
While there are many complex factors in a health system that can impact physical infrastructure, some of the major drivers are listed below. To aid in the prioritization process, we group the ‘related elements’ into:
Upstream elements
We define “upstream elements” as the factors in a health system that have the potential to make the biggest impact, whether positive or negative, on physical infrastructure.
- Policy & leadership
-
A huge driver for physical infrastructure comes down to policy and leadership at the national level. Leadership must recognize the importance of keeping physical infrastructure top of mind, as many core elements of primary health care fall downstream to physical infrastructure. Policies should work to establish target facility density and infrastructural standards to meet population health needs.
- Multi-sectoral approach
-
Another driver is priority setting. To ensure that the design, distribution, and day-to-day functions of physical infrastructure align with local needs, decision-makers should work to gather and use data on the current conditions of facilities, including what they are lacking and what they have. Decision-makers can then use this data to better allocate resources and ultimately, address gaps in the quality and availability of physical infrastructure.
Complementary elements
We define “complementary elements” as the factors in a health system that have the potential to make an impact, whether positive or negative, on the physical infrastructure. However, we consider these drivers as complementary to, but not essential to performance.
- Purchasing & payment systems
-
Purchasing and payment systems often impact the acquisition of and investment into necessary infrastructure, however, it is not necessary that spending on PHC alone would impact this input.
- Funding & allocation of resources
-
Changes to the funding and allocation of resources for PHC as a whole can impact physical infrastructure, however, similarly to purchasing and payment systems, it is not necessary that this aspect of financing alone would impact this input.
- Resilient facilities & services
-
Assessing resilience in service preparedness can help identify areas of vulnerability and opportunities for further investment in the physical infrastructure of a facility.
- Management of services
-
Adequate management of services can help to maintain the strong physical infrastructure of health facilities. Given that some facility funding is decentralized, its management can be complementary to the purchasing and maintenance of facility infrastructure. Additionally, facility performance assessments help identify potential areas for infrastructure prioritization and improvement.
- Primary care functions
-
Health facilities should be built with maximizing the patient experience in mind. Thus, person-centred care begins, in large part, with facility design. The close attention to patient-centeredness in primary health care facilities means that their design is, or should be, quite different from other kinds of health care facilities by being more in tune with the needs of diverse populations.
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Countries seeking to improve physical infrastructure can pursue a wide array of potential improvement pathways. The short case studies below highlight promising and innovative approaches that countries around the world have taken to improve.
PHCPI-authored cases were developed via an examination of the existing literature. Some also feature key learnings from in-country experts.
- East Asia & the Pacific
- Europe & Central Asia
- Latin America & the Caribbean
- Middle East & North Africa
- North America
- South Asia
- Sub-Saharan Africa
-
- Ethiopia: Strengthening Primary Health Care Systems to Increase Effective Coverage and Improve Outcomes in Ethiopia
- Ghana: Addressing transportation barriers via a community and sub-district level emergency transport system in Ghana
- Senegal: Using facility assessments to improve healthcare infrastructure
- South Africa: Making facility operations safer during the COVID-19 pandemic in South Africa
- South Africa: WASH infrastructure and practices in primary health care clinics in the rural Vhembe District municipality in South Africa
- Tanzania: Rapid assessment of infrastructure of primary health care facilities – a relevant instrument for health care systems management
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Building consensus on what strong physical infrastructure looks like and key strategies to fix gaps is an important step in the improvement process.
Below, we define some of the characteristics of strong physical infrastructure in greater detail:
-
Ensuring that all populations have timely, geographic access to care requires sufficient facility infrastructure7. The density and distribution of primary care facilities refer to the physical locations of primary care facilities and their spread relative to the population. The number and type of facilities needed in a country or region depend on two categories of factors. The first is population needs, including the burden of disease and population distribution. The second is models of care, including the availability of services at facilities, staffing of facilities, and referral expectations. Because a range of factors and needs influence and distribution, there are no specific global guidelines for making these decisions. Instead, it is important for countries to assess their own facility density and distribution needs and set targets that respond to these needs and the local context7.
Note: Geographic access from the patient perspective is explored in the Access module.
-
One of the guiding principles behind the design of health facilities is being able to meet the most common problems in a community. This is achieved in part through a close understanding of the health status and needs of community members8. Person-centred care begins in large part with facility design. The close attention to patient-centeredness in primary health care facilities means that their design is, or should be, quite different from other kinds of healthcare facilities. Facility design is a critical component to achieving high-quality, person-centred care, but is often not taken into consideration – or is thought to be a “luxury” in resource-constrained settings. Additionally, much of the research on evidence-based facility design has focused on hospitals rather than PHC settings9. However, patient-centeredness is core to PHC and needs to be included in PHC facility design from the start. Evidence has shown that patient-centred design can facilitate improved access, improve the waiting experience, privacy, and physician/staff-patient communication, reduce patient anxiety, and reduce the risk of infection.10 More on person-centred care can be found in the Primary Care Functions module.
-
Facility amenities Facility amenities are the features and utilities that enable primary care facilities to be ready and able to provide quality, person-centered primary health care. Basic amenities include electricity, safe water, exam rooms with auditory and visual privacy, light sources, sanitation facilities (toilet/latrine: flush/pour toilets to piped sewer system or septic tank, pit latrine, composting toilet), communication equipment (cell phone, landline telephone, and/or shortwave radio), computer with internet or network connectivity, and access to emergency transportation. are the most basic essential features and utilities that enable primary care facilities to be ready and able to provide quality, person-centred primary health care. Facility amenities Facility amenities are the features and utilities that enable primary care facilities to be ready and able to provide quality, person-centered primary health care. Basic amenities include electricity, safe water, exam rooms with auditory and visual privacy, light sources, sanitation facilities (toilet/latrine: flush/pour toilets to piped sewer system or septic tank, pit latrine, composting toilet), communication equipment (cell phone, landline telephone, and/or shortwave radio), computer with internet or network connectivity, and access to emergency transportation. are a core component of a health facility’s readiness to provide services11.
According to the WHO Building Blocks of Health Systems, essential facility amenities include electricity, safe water, exam rooms with privacy from sight and sound, light sources, sanitation facilities (such as a flush or pour toilets to a piped sewer system or septic tank, pit latrines, and/or composting toilets), communications equipment (such as cell phones, landline telephones, and/or shortwave radios), computers with internet or network connectivity, and access to emergency transportation.
-
Standard safety precautions Standard precautions are established processes that require health care workers to assume that the blood and body substances of all patients are potential sources of infection, regardless of the diagnosis or presumed infectious status, in order to provide a high level of protection to patients, health care workers, and visitors. Standard precautions include the following practices: hand washing and antisepsis (hand hygiene); use of personal protective equipment when handling blood, body substances, excretions, and secretions; appropriate handling of patient care equipment and soiled linen; prevention of needlestick or sharp injuries; environmental cleaning and spill management; and appropriate handling of waste 14. and equipment are the processes and materials that support safe primary care service delivery and prevent the transmission of communicable diseases. and , sometimes called standard precautions for the prevention of infections, are a core component of health facility readiness to provide high-quality services and ensure the safety of patients and providers11.
Standard safety equipment Standard safety equipment are the materials needed to support primary care service delivery and reduce the risk of transmission of bloodborne and other pathogens from both recognized and unrecognized sources. They are the basic level of infection control precautions which are to be used, as a minimum, in the care of all patients. These include basic safety tools such as sterilization equipment, safe final disposal of sharps and medical waste, sharps boxes or containers in exam rooms, waste bins with lids and liners in exam rooms, surface or environmental disinfectant, single-use standard disposable or auto-disposable syringes, bar or liquid soap along with running water or alcohol-based hand sanitizer, latex gloves, and guidelines for standard precautions against infection. and precautions include basic safety tools such as sterilization equipment, safe final disposal of sharps and medical waste, sharps boxes or containers in exam rooms, waste bins with lids and liners in exam rooms, surface or environmental disinfectant, single-use standard disposable or auto-disposable syringes, bar or liquid soap along with running water or alcohol-based hand sanitiser, latex gloves, and guidelines for standard precautions against infection711
-
As described above, gaps still remain in ensuring sufficient facility amenities, safety precautions, and equipment. Assessment tools enable decision-makers to gather information on the conditions of facilities to inform priority setting and quality improvement efforts.
Various assessment tools have been developed to measure the critical areas of service availability, readiness, and provision. As more countries take part in these assessments, the data they gather can be used to help prioritize facility infrastructure needs as specifically as in a single health care facility and as broadly as in a whole region. Researchers at The Water Institute compiled data for an array of indicators of health centre environmental conditions and standard precaution items from LMICs, representing 58% of the total population of LMICs and 129,557 health care facilities between 2007-2016. These data found that 59% of health care facilities lacked reliable energy services, 50% lacked piped water on premises, and 33% lacked improved sanitation facilities on premises12345. Further, nationally representative data from a subset of six countries showed that only 2% of health care facilities provide all four of water, sanitation, hygiene, and waste management services. There were statistically significant inequalities in coverage by urban versus rural setting, managing authority, facility type, and subnational administrative unit.6 The study also looked at indicators of environmental conditions and standards at health facilities – including water, sanitation, hygiene, energy, and waste management – and found that more than half of facilities were equipped with disposable syringes (85.2%), latex gloves (76.5%), appropriate storage of sharps waste such as sharps boxes (74.7%), disinfectant (e.g. chlorine solution for decontamination) (63.6%), safe disposal of sharps (63.6%), appropriate disposal of infectious waste (60.9%), and soap for handwashing (60.8%). Conversely, fewer than half had appropriate storage of infectious waste (39.3%), alcohol-based hand disinfectant (29.5%), sterilization equipment (26.8%), and guidelines for standard precautions (26.2%).6
See action 1 for more information on facility assessment and reporting, including relevant tools, resources, and supporting elements.
-
- Facility density The number of primary care facilities per number population. Some indicators base the facility density per 10,000 people, others by 5,000 or 100,000. : The number of primary care facilities per number population. Some indicators base the facility density per 10,000 people, others by 5,000 or 100,0001
- Master Facility List A Master Facility List is a complete listing of health facilities in a country, both public and private. It is composed of a set of administrative information and data that identifies each facility – such as facility codes, names, types, ownership or managing authority, location, address, and contact information, geographic coordinates, and operational status, as well as services offered, human resources, and infrastructure details such as number of inpatient beds – and is used as a standard mechanism for uniquely identifying health facilities and allowing for information to be compared across time and across data sources for individual facilities. : A Master Facility List A Master Facility List is a complete listing of health facilities in a country, both public and private. It is composed of a set of administrative information and data that identifies each facility – such as facility codes, names, types, ownership or managing authority, location, address, and contact information, geographic coordinates, and operational status, as well as services offered, human resources, and infrastructure details such as number of inpatient beds – and is used as a standard mechanism for uniquely identifying health facilities and allowing for information to be compared across time and across data sources for individual facilities. is a complete listing of health facilities in a country, both public and private. It is composed of a set of administrative information and data that identifies each facility – such as facility codes, names, types, ownership or managing authority, location, address, and contact information, geographic coordinates, and operational status, as well as services offered, human resources, and infrastructure details such as the number of inpatient beds – and is used as a standard mechanism for uniquely identifying health facilities and allowing for information to be compared across time and across data sources for individual facilities.12
- Standard safety equipment Standard safety equipment are the materials needed to support primary care service delivery and reduce the risk of transmission of bloodborne and other pathogens from both recognized and unrecognized sources. They are the basic level of infection control precautions which are to be used, as a minimum, in the care of all patients. These include basic safety tools such as sterilization equipment, safe final disposal of sharps and medical waste, sharps boxes or containers in exam rooms, waste bins with lids and liners in exam rooms, surface or environmental disinfectant, single-use standard disposable or auto-disposable syringes, bar or liquid soap along with running water or alcohol-based hand sanitizer, latex gloves, and guidelines for standard precautions against infection. : Standard safety equipment Standard safety equipment are the materials needed to support primary care service delivery and reduce the risk of transmission of bloodborne and other pathogens from both recognized and unrecognized sources. They are the basic level of infection control precautions which are to be used, as a minimum, in the care of all patients. These include basic safety tools such as sterilization equipment, safe final disposal of sharps and medical waste, sharps boxes or containers in exam rooms, waste bins with lids and liners in exam rooms, surface or environmental disinfectant, single-use standard disposable or auto-disposable syringes, bar or liquid soap along with running water or alcohol-based hand sanitizer, latex gloves, and guidelines for standard precautions against infection. are the materials needed to support primary care service delivery and reduce the risk of transmission of bloodborne and other pathogens from both recognized and unrecognized sources.113 They are the basic level of infection control precautions which are to be used, as a minimum, in the care of all patients.13 These include basic safety tools such as sterilization equipment, safe final disposal of sharps and medical waste, sharps boxes or containers in exam rooms, waste bins with lids and liners in exam rooms, surface or environmental disinfectant, single-use standard disposable or auto-disposable syringes, bar or liquid soap along with running water or alcohol-based hand sanitiser, latex gloves, and guidelines for standard precautions against infection.678910
- Standard safety precautions Standard precautions are established processes that require health care workers to assume that the blood and body substances of all patients are potential sources of infection, regardless of the diagnosis or presumed infectious status, in order to provide a high level of protection to patients, health care workers, and visitors. Standard precautions include the following practices: hand washing and antisepsis (hand hygiene); use of personal protective equipment when handling blood, body substances, excretions, and secretions; appropriate handling of patient care equipment and soiled linen; prevention of needlestick or sharp injuries; environmental cleaning and spill management; and appropriate handling of waste 14. : Standard precautions are established processes that require health care workers to assume that the blood and body substances of all patients are potential sources of infection, regardless of the diagnosis or presumed infectious status, in order to provide a high level of protection to patients, health care workers, and visitors.14 Standard precautions include the following practices: hand washing and antisepsis (hand hygiene); use of personal protective equipment when handling blood, body substances, excretions, and secretions; appropriate handling of patient care equipment and soiled linen; prevention of needlestick or sharp injuries; environmental cleaning and spill management; and appropriate handling of waste.14
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
References:
- The DHS Program - Service Provision Assessments (SPA). [cited 2018 Jan 21]; Available from: https://dhsprogram.com/What-We-Do/Survey-Types/SPA.cfm
- Service Delivery Indicators (SDI) | Data Catalog [Internet]. [cited 2019 Mar 15]. Available from: https://datacatalog.worldbank.org/dataset/service-delivery-indicators
- World Health Organization. WHO | Service Availability and Readiness Assessment (SARA). 2015;
- WHO. Infection Prevention and Control Assessment Framework at the Facility Level. Geneva, Switzerland: WHO; 2018.
- World Health Organization. Interim practical manual supporting implementation of the WHO Guidelines on Core Components of Infection Prevention and Control Programme. World Health Organization. 2018;
- Cronk R, Bartram J. Environmental conditions in health care facilities in low- and middle-income countries: Coverage and inequalities. Int J Hyg Environ Health. 2018 Apr;221(3):409–22.
- PHCPI. Primary Health Care Progression Model Assessment Tool [Internet]. Primary Health Care Progression Model Assessment Tool. 2019. Available from: https://improvingphc.org/sites/default/files/PHC-Progression%20Model%202019-04-04_FINAL.pdf
- Foundation C. Designing Safety-Net Clinics for Innovative Care Delivery Models. California HealthCare Foundation. 2011;
- Gunn R, Davis MM, Hall J, Heintzman J, Muench J, Smeds B, et al. Designing clinical space for the delivery of integrated behavioral health and primary care. J Am Board Fam Med. 2015 Oct;28 Suppl 1:S52-62.
- Gulwadi GB, Joseph A, Keller AB. Exploring the impact of the physical environment on patient outcomes in ambulatory care settings. HERD. 2009;2(2):21–41.
- WHO. Monitoring the Building Blocks of Health Systems: A handbook of indicators and their measurement strategies . World Health Organization; 2010.
- WHO. Transforming Vision into Action: Operational Framework for Primary Health Care. WHO; 2020 Dec.
- Tine J, Faye S, Nakhimovsky S, Hatt L. Universal Health Coverage Measurement in a Lower-Middle-Income Context: A Senegalese Case Study. Bethesda, MD: Health Finance & Governance Project: Abt Associates Inc.; 2014.
- REPUBLIQUE DU SENEGAL. Programme Développement de la Carte Sanitaire (PDCS) 2019 - 2023 . Ministère de la Santé et de l’Action Sociale. 2018;
- International Bank for Reconstruction and Development / The World Bank. Service Delivery Indicators Senegal . International Bank for Reconstruction and Development / The World Bank. 2013;
- Devlin K, Farnham Egan K, Pandit-Rajani T. COMMUNITY HEALTH SYSTEMS CATALOG COUNTRY PROFILE: SENEGAL. Community Health Systems Catalog Country Profile: Senega. 2016;
- The World Bank. Sri Lanka ‐ Second Health Sector Development Project . IMPLEMENTATION COMPLETION AND RESULTS REPORT. 2019;
- Research A for HP and S. Primary Health Care Systems (PRIMASYS) [Internet]. www.who.int. 2017. Available from: http://www.who.int/alliance-hpsr/projects/primasys/en/
- Elevating Sri Lanka’s Public Health to the Next Level [Internet]. [cited 2020 Aug 12]. Available from: https://www.worldbank.org/en/results/2018/09/14/elevating-sri-lankas-public-health-next-level
- Ministry of Health, Nutrition and Indigenous MedicineDepartment of Census and Statistics,Ministry of National Policies and Economic Affairs. Service Availability and Readiness AssessmentSri Lanka 2017. Service Availability and Readiness Assessment 2017 Sri Lanka. 2018;