By John Koku Awoonor-Williams, Elisabeth Tadiri, and Hannah Ratcliffe
The Community-based Health Planning and Services (CHPS) initiative in Ghana was created in 1994 with the aim of reducing barriers to geographical access to health care. This initiative is an evidence-based approach to providing community-based care to underserved populations through training and deploying nurses as Community Health Officers (CHOs). These nurses provide door-to-door services for the catchment area of their “CHPS zone,” as well as basic services at community-based CHPS compounds. The CHPS model is based on the premise that community engagement is both a critical function and enabler of strong primary health care systems.
After preliminary success with an experimental trial in Navrongo in the Upper East Region during the early 1990s, CHPS became a part of the national health policy in Ghana in 1999. National scale-up of the CHPS model occurred gradually (Figure 1), and the Ghana Health Services (GHS) took advantage of the incremental rollout to conduct implementation research to identify the most effective components of the model. This careful study has led GHS to conclude that community engagement and participation are the most critical components of CHPS for ensuring effective primary health care, and where these components were neglected in the rollout of CHPS, the model has struggled to take hold and health outcomes have not been as positive as desired.
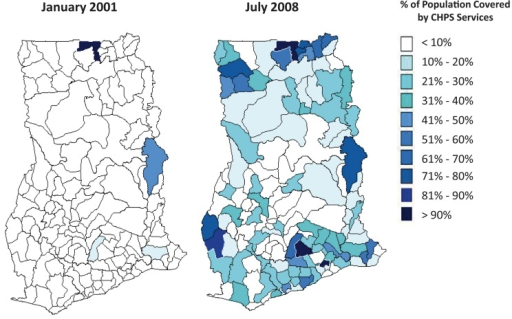
Figure 1: Scale-up of Community-based Health Planning and Services model (CHPS) in Ghana from 2001 to 2008. Source: Awoonor-Williams et al. (2013) Lessons learned from scaling up a community-based health program in the Upper East Region of northern Ghana. Global Health Science and Practice. 1(1):117-133.
 Photo: Columbia University
Photo: Columbia University
A major part of the implementation guide will be the "15 Steps and Milestones for CHPS Implementation," which draw on lessons learned from the last 20 years of CHPS implementation to explicitly set forth the steps needed to properly and adequately engage communities and create a critical cohort of community health volunteers. These steps are tied to a set of specific activities, for example: situation analysis and problem identification with district teams, sensitization of health workers to the CHPS model, community outreach events such as durbars (traditional festive gatherings), selection of sites for CHPS compounds, and selection and training of Community Health Management Committees (CHMC). Research has shown that the successful completion of every step is critical to the success of CHPS zones, so each of the 15 Steps identifies a set of deliverables to ensure completion of all activities, as well as an individual or group who is responsible for implementation to ensure accountability. Clearly linking all the steps to the ultimate goal enables participants to see the value in working sequentially. Furthermore, the 15 Steps are organized into 6 Milestones to encourage a sense of accomplishment and progress within the district health management team (DHMT), as well as the community.
Throughout the process of scaling CHPS, Ghana has employed a “District of Excellence” model to promote intra-country learning and peer-to-peer sharing. In this model, teams from districts about to begin the process of establishing a CHPS zone can participate in a week-long observation and training course at a “District of Excellence” CHPS zone selected for its model leadership and system 
Ghana has long been seen as a leader in health systems performance in sub-Saharan Africa. Previous work on the CHPS strategy has informed primary health care reforms in Ethiopia, Burkina Faso, Tanzania, Nigeria, and Sierra Leone. With the new CHPS reforms, Ghana is again setting an example and drawing attention to the critical role of community engagement and participation in ensuring the success of PHC systems.
To learn more about CHPS, visit their website at http://www.ghanahealthservice.org/chps.
John Koku Awoonor-Williams MD, MPH, PhD, is Director of the Ghana Health Service Policy Planning Monitoring and Evaluation Division. Dr. Awoonor-Williams’ expertise includes health systems development, expanding access to healthcare for rural marginalized populations and emergency obstetric referral services
Elisabeth Tadiri is a Primary Health Care Intern at Ariadne Labs, a joint center between Brigham and Women’s Hospital and the Harvard T. H Chan School of Public Health.
Hannah Ratcliffe, MSc is a Primary Health Care Research Specialist at Ariadne Labs.
