By Elizabeth Annis and Hannah Ratcliffe
In 1993, Ethiopia instituted a new National Health Policy to improve overall health status by increasing access to primary health care services throughout the country. This policy—coupled with Ethiopia’s commitment to system improvement—led to a twenty-year, four-stage Health Sector Development Plan (HSDP) that was in place from 1995 to 2015 and resulted in major reforms across the Ethiopian health system. Phases I and II of the HSDP were in place from 1997-2005 with the ambitious focus of improving health service delivery and quality of care; health facility rehabilitation and expansion; human resource development; pharmaceutical supply and management; information, education, and communication; health sector management; health management information systems; and health care financing.(1) Phase III of the HSDP ran from 2005 to 2010 and focused on improving maternal and child health and addressing communicable diseases.
The Health Extension Program (HEP) was launched in 2003 under HSDP II and continued under HSDP III with the mission to “deliver health promotion, disease prevention, and selected curative health services at the community level” to achieve universal primary health care coverage.(2,3) Since 2003, the HEP and HSDP have dramatically reformed the Ethiopian health care system, and the primary health care system in particular. The reforms initiated under these programs have touched on nearly all aspects of the PHCPI Conceptual Framework—from systems and inputs to service delivery to outcomes and outputs—and the following case study highlights the reforms initiated through and impact achieved by these programs.

System: Governance and Health Financing
The Health Sector Development Plan decentralized management of the public health system and distributed responsibility to the Regional Health Bureau (RHB) level in an effort to improve effectiveness, efficiency, equity, and sustainability.(2) These reorganizational decisions allowed RHBs to distribute authority and management power even further to the local level to foster more community engagement. To ensure proper processes and provide necessary leadership, the Government of Ethiopia and the Federal Ministry of Health established a joint Steering Committee between the Federal Ministry of Health and the Regional Health Bureaus, a Joint Consultative Forum, and the Joint Core Coordinating Committee to oversee the implementation of HSDP.(2)
The HSDP also introduced financing reform efforts, and from 2007 to 2011, spending on health care increased from 4.5% to 5.2% of Ethiopia’s GDP.(2) In general, these spending adjustments contributed to increases in health resources, support for low-income communities, and the establishment of financial mechanisms. As a result, the government also created a community-based health insurance (CBHI) and social health insurance (SHI). These insurance systems aim to expand financial coverage, with support from government funding and the existing Ethiopian Health Insurance Agency (EHIA). Overall, the goal is for these insurance programs to contribute to the establishment of universal health coverage in Ethiopia, though current insurance coverage remains quite low at approximately 4%.(4)
Inputs: Development of Primary Health Care Units and Health Extension Workers
The health system in Ethiopia is structured into three tiers (Figure 1). National referral hospitals provide specialized services; regional referral hospitals in each of Ethiopia’s nine regions provide general referral services; and primary health care units (PHCU) operate at the woreda (district) and kebele (lowest administrative level) to provide primary health care services to communities.(5) In rural areas, PHCUs are comprised of five health posts (one per kebele) which report to one health center at the woreda level, which in turn reports to a primary hospital. In urban areas, primary health care units are typically health centers. To expand access to care, the HEP coordinated a major expansion in the number of health facilities that make up PHCUs. By 2015, Ethiopia had newly built 16440 health posts; 3547 health centers; and 311 hospitals.(6)
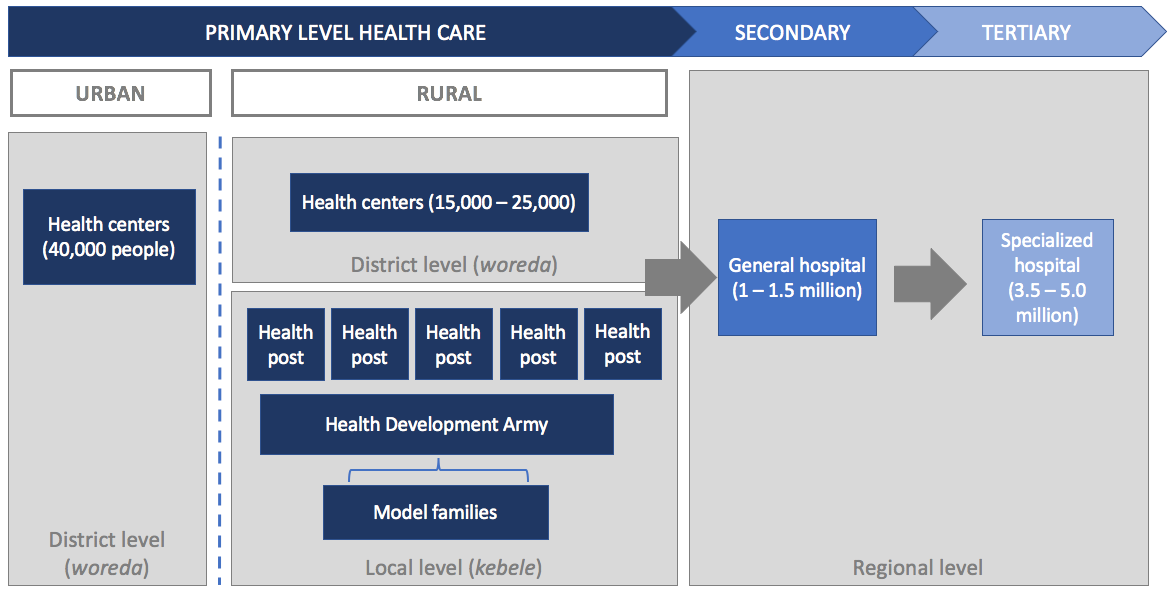 Figure 1: Structure of Ethiopian health system
Figure 1: Structure of Ethiopian health system
A second core component of the HEP was to strengthen human resources for health, which it did through the creation of a new cadre of health workforce—the Health Extension Worker (HEW). HEWs are frontline, community-based health care workers tasked with providing 16 packages of promotive, preventive, and selected curative services focused on four areas: promotion of hygiene and environment sanitation, prevention and control of major communicable diseases, promoting and providing family health services, and health education and communication.(2) By May 2009, the Federal Ministry of Health had trained over 30,000 new HEWs, and it is estimated that over 38,000 HEWs are now working in Ethiopia.(3,7) Health Extension Workers are women recruited from their communities and trained in regionally based institutes for one year on the essential package of services they are expected to provide.(6) After training, HEWs are deployed to health posts. Each health post is staffed with two HEWs, who are expected to split their time between the health post and their community. In the health post, HEWs provide family planning, maternity services, immunizations, and nutrition counseling, and refer more complicated health needs to health centers and hospitals.(8) When out in the community, HEWs provide basic promotive and preventive services, offer health education, and collect vital statistics.(9)
To complement these expansions of the health workforce and facility infrastructure, Ethiopia introduced new information systems, including a system that ensures continuous availability of drugs and supplies. In 2007, Ethiopia founded the Pharmaceutical Fund and Supply Agency (PFSA) to manage the country’s supply chain and determine strategic plans to improve availability of medicines throughout the country. In 2010, PFSA implemented the Integrated Pharmaceuticals Logistics System (IPLS) to improve the management of pharmaceutical supplies through more refined record keeping, storage, and availability. IPLS provided trainings to improve communication between supervisors and suppliers in order to better monitor supplies stocks. By 2014, availability of essential medicines increased from 65% to 89%, nearly reaching the HSDP goal of 100%.(2) To extend these efforts, Ethiopia is working to expand its warehouse and cold chain capacity for storing and distributing pharmaceuticals, and has introduced larger trucks to distribute supplies in an integrated supply chain.(2) Health facilities at all levels are now able to monitor their supply and demand and adjust supply requests accordingly.
Service Delivery: Population Health Management
The HSDP and HEP placed enormous importance on community engagement and proactive population outreach. Through PHCUs and the deployment of health extension workers, the HEP created a system of geographic empanelment, wherein every health post is responsible for a population of approximately 5000 people. Under this system communities have a dedicated first point of contact with the health care system and health workers are accountable for the health status of their geographically empaneled communities.
Additionally, to increase community engagement, a key responsibility for Health Extension Workers is to train “model families” who can help spread health education within their communities. Model families in turn make up the Health Development Army, which aims to “engage community, identify locally salient bottlenecks that hinder uptake of services, and scale up best practices.”(Figure 1) (2) By 2014, there were 442,773 Health Development Army groups, each comprised of 30 households.(2) Together, Health Extension Workers and the Health Development Army provide a platform for proactive population outreach and local priority setting based on relevant data collected from within the community.
Access
The HSDP and HEP have improved financial, geographic, and timely access to care in Ethiopia. The expansion of the number of facilities and amount of community outreach have improved geographic access to care, particularly for poor and rural populations.(10) Community-based health insurance and social insurance schemes have reduced out-of-pocket costs for both formally and informally-employed populations.(2) By 2020, Ethiopia aims to enroll 80% of households in 80% of all woredas in CBHI and cover the entire formal sector with SHI.
Facility Organization and Management
In 2005 and 2006, under the HSDP, facility governing boards were introduced to improve decision-making and responsiveness to communities. In practice, these governing boards approve the health facility plan and budget, manage revenue decisions, and evaluate facility performance.(11) As of 2015, 93.3% of all health centers had established governing boards, and an assessment found that approximately half of all hospital and health center governing boards met on a monthly basis.(2)
To further support performance measurement and management, in 2008 Ethiopia implemented a new Health Management Information System (HMIS). By the end of Ethiopian 2013, the HMIS system had been implemented in 98% of public hospitals and in 87% of health centers. Additionally, over 60% of facilities staffed a full-time HMIS focal person, enabling improvements in completeness and timeliness of health reports.(2) Subsequently Ethiopia introduced a new Woreda Based Planning process that utilizes the facility-level data now available via HMIS to plan future spending and management according to facility-specific needs.(2) Through the Woreda Based Planning system, stakeholders as diverse as community leaders, development partners, non-governmental organizations, and health center managers jointly plan service priorities in order to align and harmonize planning, budgeting, resource allocation, and reporting systems.
At the hospital level, Ethiopian has undertaken substantial efforts to improve management and performance, including the Ethiopian Health Reform Implementation Guidelines (EHRIG) and the Ethiopian Hospital Alliance for Quality (EHAQ). The EHRIG outlines 124 management standards for hospitals regarding the following functions: leadership and governance, patient flow, medical records management, pharmacy services, laboratory services, nursing care, infection prevention, facilities management, medical equipment management, financial and asset management, human resource management, quality management, and monitoring and reporting.(11) Hospitals report on each standard on a quarterly basis, and performance has improved quickly over time: a 2015 study shows that from 2011 to 2014, the percentage of government hospitals regularly reporting their performance increased from 40% to 84%.(11)
The EHAQ is a national quality improvement collaborative that includes all hospitals in Ethiopia, and has focused on improving patient experience of care and the quality of maternal, neonatal, and child health services.(12) EHAQ analyzes data generated by the EHRIG related to a particular area of focus; for hospitals that do not meet EHRIG standards, EHAQ provides information regarding techniques and approaches to improve performance. Hospitals are also grouped into clusters with one “mentor” hospital, which provides the opportunity to learn from each other. A recent study showed that the process of implementing EHAQ and EHRIG led to a 10% increase in patient satisfaction at hospitals from 2012 to 2014, with hospital clusters that reported sharing knowledge with each other seeing greater improvements that those that did not.(12)
These efforts at the hospital level have been supported by Ethiopian Hospital Management Initiative, a collaboration between the Clinton Health Access Initiative, Yale University, and the Federal Ministry of Health.(11–15) The Initiative established a partnership-mentorship program to build management capacity in hospitals through a yearlong fellowship program and training for hospital management teams through the Yale Professional Development Program in International Health Care Management and a masters degree program in Healthcare and Hospital Administration for hospital CEOs.(14) One evaluation of the program found that participating hospitals improved on 60% of EHRIG standards, including those on human resources, medical records and patient flow, nursing standards and practice, infection prevention and control, quality management and financial management.(15)

This range of initiatives and programs, stemming from the Health Extension Program, has contributed to improvements in service coverage and health outcomes. For example, from 2000 to 2016, antenatal care (ANC) coverage increased from 27% to 62%, while effective coverage (at least four ANC visits) increased from 10% to 32%.(4) Similarly, facility-based delivery rates increased from 5% in 2000 to 26% in 2016, and skilled assistance during delivery increased from 6% to 28% during the same period. Basic vaccination coverage rates have increased from 14% in 2000 to 39% in 2016, and the percent of children with diarrhea receiving appropriate care increased from 13% to 44%. Additionally, studies have documented a specific link between the intensity of Health Extension Program and Health Development Army implementation and coverage of key maternal and child health services.(16,17)
Health outcomes have also improved significantly. Under-5 mortality rates declined from 166 deaths per 1000 live births in 2000 to 67 in 2016. Infant and neonatal mortality rates have also declined, though less quickly than under-5 mortality overall. Finally, the probability of dying between ages 15 and 50 has declined by more than 50% since the year 2000, from 221 per 1000 women to 100 per 1000 women and from 275 per 1000 men to 124 per 1000 men.
Despite these improvements, challenges in achieving effective coverage still remain. For example, met need for family planning in 2016 was only 36% and only 17% of women received a postnatal care visit within two days of childbirth, indicating continued progress is needed to ensure continuity and comprehensiveness of services. Additionally, stark disparities persist in access to care and health outcomes between urban and rural populations and across educational achievement levels of women.
Looking Forward
In 2015, at the conclusion of the Health Sector Development Plan IV, Ethiopia introduced the Health Sector Transformation Plan (HSTP)—the first phase of a second twenty-year strategy known as “Envisioning Ethiopia’s Path to Universal Health Care through strengthening of Primary Health Care.” The HSTP targets quality and equity, universal health coverage, and transformation of the health system through a series of initiatives related to interventions for reproductive, maternal, newborn, child and adolescent health; nutrition; communicable and non-communicable diseases (NCD); health emergency risk management; community engagement and ownership; improvements in efficiency and effectiveness through financial management; socio-economic development; governance; and regulations.(2) Ethiopia has outlined specific interim health status goals for 2020: reduce maternal mortality ratio to 199/100,000 live births; reduce under-5 mortality to 30, infant mortality to 20, and neonatal mortality to 10 per 1,000 live births; reduce stunting to 26%, wasting to 4.9%, and underweight to 13%; reduce HIV by 60% and eliminate new infections in children; reduce tuberculosis deaths by 35% and incidence by 20%; reduce malaria incidence and mortality by 40% each; and stabilize and reduce deaths/injuries from road accidents.(2)
One method Ethiopia is employing to reach these ambitious targets is the creation of model kebeles as an extension of the model families and Health Development Army initiative.(18) These networks of model families are intended to further strengthen proactive population outreach and help identify local health needs and promote interventions in order to build on the successes of the HDA and improve the comprehensiveness of care delivery. Kebeles will be identified as models based on repeated evaluations with the goal of obtaining 80% model villages by 2020. To complement these model kebeles, community-based health insurance will be expanded to increase financial access.
Building on the platform established by the HSDP, under the HSTP Ethiopia is seeking to expand coverage beyond communicable disease and maternal and child health programs to address mental health, non-communicable diseases, and family medicine. For example, the HSTP established the national goal of ensuring that every woreda has access to mental health services by 2020.(19) Achievement of this goal will be supported through a National Mental Health Strategy and the Programme for Improving Mental Healthcare. (20) These efforts aim to improve equitable access to care by integrating mental health services into primary health care and training frontline providers to deliver mental health care services and treat psychosis, depression, epilepsy, and alcohol use disorders.(19,21)
Similarly, Ethiopia has developed a National Strategy Action Plan for Prevention and Control of NCDs, which launched in 2014.(22) This strategy entails expanding primary health care service packages to include interventions that target NCDs, such as screenings and vaccinations, and supporting human resource strengthening to ensure services are delivered to defined standards. The introduction of these new services into primary health care will require strengthening available human resources. To do so, the role of family medicine doctors is being promoted in Ethiopia. In 2013, Addis Ababa University initiated the first family medicine residency program and the first class of residents graduated in 2016. Since then, the Federal Ministry of Health has increased recruitment of family medicine residents and introduced additional residency programs at two other universities.
Conclusion
Ethiopia has demonstrated a strong and enduring commitment to health systems strengthening through improved primary health care service delivery. Through the Health Sector Development Plan, Ethiopia implemented major reforms to improve governance, financing, inputs, and service delivery, with a particular emphasis on proactive population health management. These efforts have established a strong foundation and laid the groundwork for Ethiopia’s pivot under the Health Sector Transformation Plan to focus on improving quality and the key functions of primary health care, including continuity, comprehensiveness, coordination, and person-centeredness, that are necessary for primary health care systems of the future.
References
1. El-Saharty S, Kebede S, Dubusho PO, Siadat B. Ethiopia: Improving Health Service Delivery. HNP Discussion Paper. 2009.
2. Ethiopian Federal Ministry of Health. Health Sector Transformation Plan (2015/16-2019/20). 2015.
3. Koblinsky M, Tain F, Gaym A, Karim A, Carnell M, Tesfaye S. Responding to the maternal health care challenge: The Ethiopian Health Extension Program. Ethiop J Heal Dev. 2010;24(SPEC. ISSUE 1):105–9.
4. Central Statistical Agency (Ethiopia), ICF Macro. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia and Rockville, Maryland, USA; 2017.
5. Ethiopia Federal Ministry of Health. Health Sector Development Programme HSDP II: 2002/03-2004/05. Report of the final evaluation of the HSDP II. 2006.
6. Abrahim O, Linnander E, Mohammed H, Fetene N, Bradley E. A Patient-Centered Understanding of the Referral System in Ethiopian Primary Health Care Units. PLoS One. Public Library of Science; 2015 Jan 5;10(10):e0139024.
7. Fetene N, Linnander E, Fekadu B, Alemu H, Omer H, Canavan M, et al. The Ethiopian Health Extension Program and Variation in Health Systems Performance: What Matters? PLoS One. United States; 2016;11(5):e0156438.
8. USAID. Essential Services for Health in Ethiopia. 2008.
9. Girma S, Yohannes A, Kitaw Y, Ye-Ebiyo Y, Seyoum A, Desta H, et al. Human Resource Development for Health in Ethiopia: Challenges of Achieving the Millennium Development Goals. Ethiop J Heal Dev. 2007;21(3).
10. Memirie ST, Verguet S, Norheim OF, Levin C, Johansson KA. Inequalities in utilization of maternal and child health services in Ethiopia: the role of primary health care. BMC Health Serv Res. BMC Health Services Research; 2016;16(1):51.
11. McNatt Z, Linnander E, Endeshaw A, Tatek D, Conteh D, Bradley EH. A national system for monitoring the performance of hospitals in Ethiopia. Bull World Health Organ. 2015;93(10):719–26.
12. Linnander E, McNatt Z, Sipsma H, Tatek D, Abebe Y, Endeshaw A, et al. Use of a national collaborative to improve hospital quality in a low-income setting. Int Health. 2015;8(2):148–53.
13. Hartwig K, Pashman J, Cherlin E, Dale M, Callaway M, Czaplinski C, et al. Hospital Management in the context of health sector reform: a planning model in Ethiopia. Int J Health Plann Manage. 2008;23:203–18.
14. Kebede S, Mantopoulos J, Ramanadhan S, Cherlin E, Gebeyehu M, Lawson R, et al. Educating leaders in hospital management: A pre-post study in Ethiopian hospitals. Glob Public Health. 2012;7(2):164–74.
15. Bradley E, Hartwig K a, Rowe L a, Cherlin EJ, Pashman J, Wong REX, et al. Hospital quality improvement in Ethiopia : a partnership – mentoring model. Int J Qual Heal Care. 2008;20(6):392–9.
16. Betemariam W, Damtew Z, Tesfaye C, Fesseha N, Karim AM. Effect of Ethiopia’s Health Development Army on maternal and newborn health care practices: A multi-level cross-sectional analysis. Ann Glob Heal. Elsevier Inc; 2017;83(1):24.
17. Karim AM, Admassu K, Schellenberg J, Alemu H, Getachew N, Ameha A, et al. Effect of Ethiopia’s Health Extension Program on Maternal and Newborn Health Care Practices in 101 Rural Districts: A Dose-Response Study. PLoS One. 2013;8(6).
18. Admasu K, Balcha T, Getahun H. Model villages: A platform for community-based primary health care. Lancet Glob Heal. World Health Organization; 2016;4(2):e78–9.
19. Mugisha J, Abdulmalik J, Hanlon C, Petersen I, Lund C, Upadhaya N, et al. Health systems context(s) for integrating mental health into primary health care in six Emerald countries: a situation analysis. Int J Ment Health Syst. England: BioMed Central; 2017;11(1):7.
20. Johansson KA, Strand KB, Fekadu A, Chisholm D. Health Gains and Financial Protection Provided by the Ethiopian Mental Health Strategy: an Extended Cost-Effectiveness Analysis. Health Policy Plan. 2016;(October 2016):czw134.
21. Hailemariam M, Fekadu A, Selamu M, Medhin G, Prince M, Hanlon C. Equitable access to integrated primary mental healthcare for people with severe mental disorders in Ethiopia: a formative study. Int J Equity Health. International Journal for Equity in Health; 2016;15(1):121.
22. Federal Ministry of Health Ethiopia. NATIONAL STRATEGIC ACTION PLAN (NSAP) FOR PREVENTION & CONTROL OF NON-COMMUNICABLE DISEASES IN ETHIOPIA 2014-2016. 2014.
