PHCPI Data Insight: ANC Coverage and Continuity Highlight Complex Issues Affecting Primary Care Services
It is widely documented that antenatal care (ANC) provides women with information on health behaviors for pregnancy and childbirth, risks and warning signs, contacts and procedures in case of problems, and help planning for a safe delivery. Additionally, ANC may also contribute to the development of relationships between women and the public health system and providers. However, ANC services are largely unavailable or underutilized in many low- and middle-income countries (LMICs).
Reducing maternal mortality is a key target of UN Sustainable Development Goal #3, and primary health care (PHC) services such as antenatal care (ANC) form the foundation for achieving this goal.
To better understand the overall performance of a primary health care system, and assess continuity of care within a system, we can measure the gap between women who complete the full course of ANC, and those who do not.
How do we measure coverage and continuity?
PHCPI uses two indicators to measure ANC effective coverage and continuity. The first, Antenatal care coverage (4+ visits) (ANC4+), measures the percent of women with a live birth who received the WHO-recommended four or more antenatal care visits over the course of their pregnancy. It is important to note that this indicator does not provide information about the content or quality of ANC visits, though these are essential factors of effective coverage. The second, Continuity of care: Antenatal care dropout rate, measures the proportion of women who initiated antenatal care (ANC) but did not complete the recommended four visits.
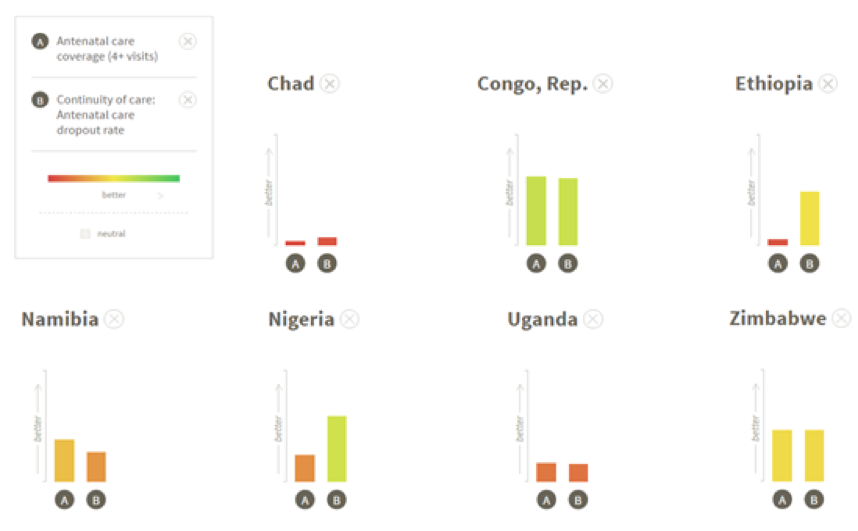
We might expect that these indicators would trend together—that is, that countries with high ANC4+ rates would have low ANC dropout rates. Using the PHCPI Compare Tool we can see that this hypothesis is often true—see, for example, Chad, Republic of Congo, Uganda, and Zimbabwe. However, there are a few countries that deviate from the norm. Exploring these cases may provide interesting insights into improving ANC effective coverage and continuity.
Deep Dive: Using the PHCPI Tool to explore ANC in the Africa Region
Ethiopia and Nigeria are both countries in which ANC4+ coverage is low, but ANC dropout rates are comparably much better. This implies that both countries have difficulty engaging women early and effectively in antenatal care but, once a woman does initiate ANC, she is likely to complete the recommended visits. This may be because relatively privileged populations in each country are able to access and continue to engage with ANC, while poorer, more rural, and/or less educated populations are unable to, unaware of, or uninterested in accessing these services. Alternatively, it could imply that once women initiate ANC, they find ANC services useful, respectful, and effective, helping them to ensure future utilization.
Countries such as Ethiopia and Nigeria may offer lessons for other countries in how to improve continuity and retention in care, but their low ANC4+ completion rates likely indicate that ANC access and utilization are highly inequitable and need to be improved.
Countries such as Namibia present a contrasting case. In Namibia, the ANC4+ coverage rate is comparatively outperforming the ANC dropout rate. Together, these indicators suggest that a very high percentage of pregnant women in Namibia access antenatal care services at least once, but continuity and retention are relatively low. Thus, in contrast to Ethiopia or Nigeria, to improve ANC coverage and continuity, Namibia would need to focus less on increasing the number of women who initiate ANC and more on retaining women in care—by, for example, better demonstrating the value of ANC services, improving clinicians’ ability to track and monitor patients over place and time, or providing more respectful, accessible, or affordable care (Finlayson 2013).
One of the expected benefits of high ANC4+ coverage is that it will translate to high rate of high-quality facility-based delivery rates (Kearns 2015). Globally, facility-based deliveries are promoted as a means of reducing maternal mortality and morbidity by increasing the likelihood that women deliver with a skilled birth attendant and are connected to a referral system. In addition to comparing ANC4+ coverage and ANC dropout rates, the PHCPI website allows us to simultaneously look at facility-based delivery rates to see how this key indicator varies with ANC coverage.
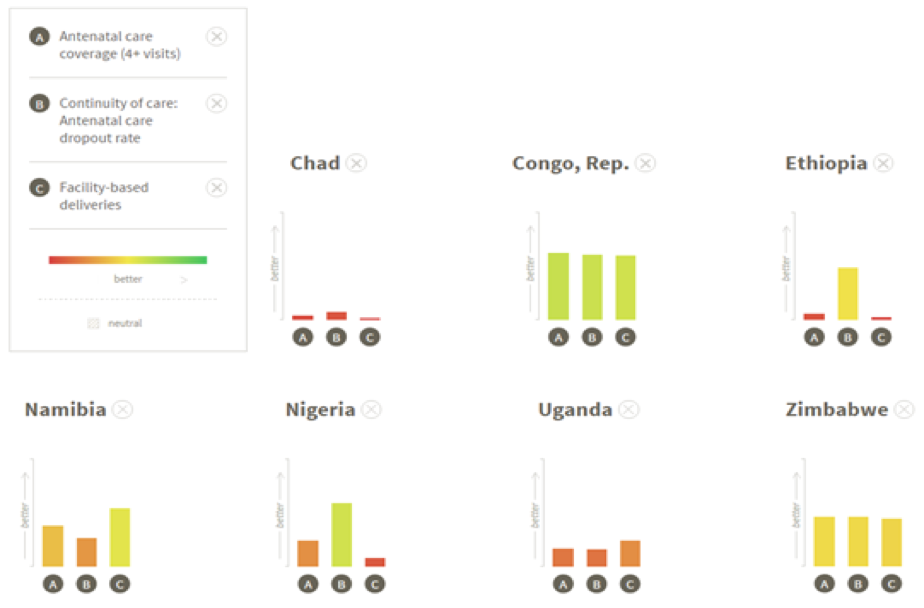
As before, many countries—including Chad, the Republic of Congo, Uganda, and Zimbabwe—exemplify the expected correlation between ANC coverage and continuity and facility-based delivery rates. The discordant cases discussed above, however, offer interesting insights into how issues of care initiation, continuity, and retention impact facility-based delivery service coverage.
What can we learn from the available data?
In Nigeria and Ethiopia, facility-based delivery rates are similar to what we might have hypothesized given the discussion above. In both countries, despite low ANC dropout rates, ANC4+ coverage is low, and so are facility-based delivery rates. We can hypothesize that it is likely the same women completing ANC4+ who are giving birth in a facility, underscoring the likelihood that both countries are able to reach only a very small percentage of pregnant women with maternal health services, and the need to expand access to, demand for, and awareness of maternal health services to improve maternal health equity.
In Namibia, the facility-based delivery rate is slightly higher than we might have expected given the ANC4+ coverage and ANC dropout rates. This may confirm our hypothesis above, that the majority of pregnant women in Namibia access at least some antenatal care, though with relatively low retention through ANC4. However, the better than expected facility-based delivery rate may indicate that this base level of ANC coverage was sufficient to help educate women on the importance of a facility-based delivery, aid them in creating a safe delivery plan, or establish at least a preliminary relationship between the woman and her family and the health care system. Yet, because the ANC4+ rates are low, women still may not be getting all the care that they need during pregnancy.
Though more analysis is needed, the data available on the PHCPI website highlight the complex factors that impact coverage and continuity of key primary care services such as maternal health care. This comparative analysis highlights opportunities for countries to learn from the successes of their peers to promote more continuous care and increase equity in access to essential services.
Hannah Ratcliffe is a Research Analyst at Ariadne Labs, a joint center between Brigham and Women’s Hospital and the Harvard T. H Chan School of Public Health.
Elisabeth Tadiri is a Primary Health Care Intern at Ariadne Labs, , a joint center between Brigham and Women’s Hospital and the Harvard T. H Chan School of Public Health.
