Data Insight
PHCPI Data Insight: Ending Preventable Maternal and Child Deaths
 World Bank/Stephan Gladieu
World Bank/Stephan Gladieu
Countries around the world have made considerable progress toward realizing this vision. Under Millennium Development Goal (MDG) 5, maternal mortality fell by 44% worldwide. Under-five mortality dropped from 91 deaths per 1,000 live births to 43 within the same time period, though it fell short of achieving the two-thirds reduction aspired to in MDG 4.
While laudable, this progress has not been enough to ensure healthy lives for women and children worldwide, and in many countries death rates remain unacceptably high. In 2015, over 300,000 women died from preventable causes related to pregnancy and childbirth. In that year alone, 5.9 million children under the age of five died, many from malnutrition and treatable diseases such as malaria, pneumonia, and diarrhea—approximately 16,000 each day. Of these, 2.7 million were newborns within their first month of life.
We know that many of these deaths are preventable. We also know which simple and affordable interventions can save the life of a mother, newborn, or child. But too often missing are the strong primary health care (PHC) systems needed to deliver those interventions in an effective and equitable way. With 99% of maternal deaths occurring in developing countries—and most maternal and child deaths happening in poor and rural communities—it’s time for the global community to take a closer look at PHC systems and how they can support the health of all women and children, everywhere.
The Role of Strong PHC Systems
Strong PHC systems improve maternal, newborn, and child health by providing the delivery platform for an integrated package of interventions within communities, supported by strong referral systems and skilled health care providers. A mother can greatly increase her baby’s and her own chances of survival when she has access to a strong, people-centered system that provides comprehensive, continuous, coordinated, and high-quality care—from family planning and antenatal care, to skilled birth attendance with referral linkages to emergency obstetric services, to postnatal care and interventions to address common childhood illnesses.
For example, the PHC Vital Signs show us that maternal mortality ratios in Sub-Saharan Africa—where over half of maternal deaths occur—are often (though not always) lower when rates of antenatal care coverage and facility-based deliveries are higher. Antenatal care coverage (4+ visits) indicates women’s access to and use of PHC services, representing opportunities for pregnant women to receive essential services vital to their health and wellbeing and that of their infants. Facility-based deliveries measures the percent of live births taking place in a public or private health facility, which can help to reduce maternal and neonatal mortality by increasing the likelihood that women deliver with a skilled birth attendant and are connected to a referral system in case of complications.
Of course, we can’t directly attribute changes in maternal mortality to these factors alone—in part because the variability in correlation across countries raises a number of questions. For instance, in the Republic of the Congo, where 79% of women receive four or more antenatal care visits and nearly 92% deliver in health facilities, maternal mortality remains high at 410 deaths per 100,000 live births. On the other hand, in Liberia, antenatal care coverage is relatively high at 78%, but only 56% of women deliver in health facilities and the maternal mortality ratio is very high at 640 deaths per 100,000 live births.
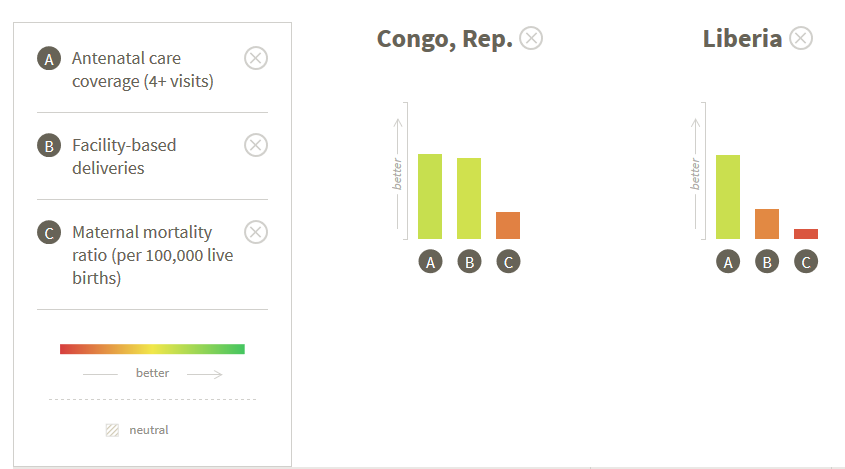
While women in the Republic of the Congo seem to have access to the health system, a number of factors may affect the quality of care that they receive. Do health facilities have insufficient human resources or high provider absence rates, resulting in timeliness delays at the point of care? Do providers face challenges of low competency, or issues of motivation and burnout in the face of high caseloads? Or do facilities lack the basic equipment and essential drugs needed to provide quality care? In Liberia, are there cultural factors inhibiting facility-based births, or do perceptions of poor quality or mistreatment deter women from delivering their babies in facilities? To answer these questions, we need more and better data to pinpoint the issues in service delivery that impact women’s access to and utilization of services, as well as their experience with the system and the quality of care provided.
Strong PHC Systems Provide Continuity of Care
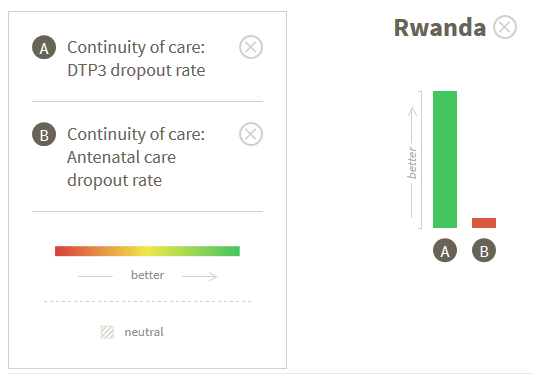
Let’s take a look at indicators of continuity of care, a key characteristic of high-performing PHC systems crucial for improved maternal and child health that reflects how patients experience health care over time. Strong PHC systems build reliable and participatory relationships between patients and health workers, where information on past events and personal circumstances is used to make care appropriate for each individual and services received from different providers are timely and complementary. For the woman we introduced in the opening paragraph, this means that the health worker she saw during her second pregnancy was the same who provided care during her first, and ensured that other providers in the hospital where she delivered her baby were aware of her pre-existing conditions.
Measuring the percent of children who do not return for the required three doses of DTP vaccine and the percent of women who do not complete four antenatal care visits before delivery, respectively, DTP3 and antenatal care dropout rates reflect the system’s ability to capture and follow up with patients and act as proxy indicators for continuity of care. In a country like Rwanda, where the DTP3 dropout rate is 0% but over half (55.7%) of pregnant women drop out of antenatal care, there are unexplained discrepancies in how the same system can achieve such different continuity outcomes between immunization and maternal care. While there may be strong immunization programs that can actively track and deliver on a child’s vaccination schedule over time, the system may simultaneously face challenges in encouraging women to seek early antenatal care and reaching them multiple times throughout their pregnancy. This lack of correlation potentially points to problems in the integration of vertical programs, and underscores the need for a strong PHC system as the vehicle that provides continuous, high-quality care for women and children from the antenatal period through the first years of life.
As countries now turn toward the achievement of universal health coverage and the other health-related Sustainable Development Goals—three targets of which relate to maternal, newborn, and child health—we need more and better data on PHC to show us where the system is working well, and where it isn’t, in order to drive improvements. Expanding measurement and promoting the use of data for PHC system improvement will be an important pathway for the global community to end preventable maternal, newborn, and child deaths by 2030 and ensure that all women and children, everywhere, have the chance to lead healthy lives.
Chloe Lanzara is a Senior Program Associate at Results for Development.
