Data Insight
PHCPI Data Insight: Health Workforce
Across the globe, over 400 million people do not have access to quality health services. One significant cause of this is a shortage of health workers – the World Health Organization estimates that an additional 4.3 million health workers are needed worldwide.
However, evidence shows that simply increasing the number of health workers is a necessary but insufficient step to ensuring quality health services for all. In addition to significant workforce shortages, countries also often lack performance data about important processes required to convert health system inputs, such as health workers, equipment, and supplies, to high-quality care delivery and coverage outputs critical to producing improved and equitable individual and population health. For example, health system managers usually don’t have good data on how often health workers are present in facilities and how accurately they diagnose and treat patients. The Primary Health Care Performance Initiative (PHCPI) calls such processes and experiences the “black box” of primary health care (PHC) because they are often not well understood and have not received enough attention.
To help shine a light on the black box, PHCPI publishes data from Service Delivery Indicators (SDI), an initiative that collects actionable data on service delivery in health facilities. These new data reveal information on aspects of the health workforce – such as provider absence, competence, and effort – that, while not often measured, are crucial for understanding health services access and quality of care, as well as the experiences of patients and providers. While limited (SDI data are currently only available in 7 countries in Sub-Saharan Africa), the data we do have provide insight into service delivery performance across and within these countries.
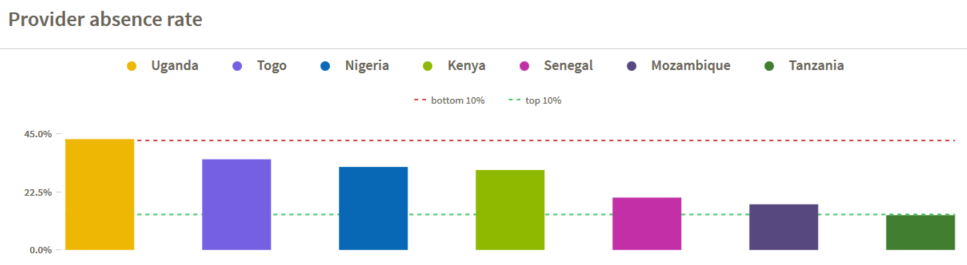
For example, when a patient enters a health facility, is a health worker present? Provider absence rate measures the number of clinical staff actually present at a facility compared to the expected number of staff at a given time. Data reveal startlingly high absence rates in some countries – in Uganda, providers are absent 43% of the time, raising important questions about potential underlying challenges in management and accountability. In particular, employment conditions, remuneration and non-financial incentives must assure fair terms for health workers, career development opportunities, and a positive practice environment to increase retention and motivation to deliver quality care. Does Uganda face greater challenges in ensuring provider presence through its current organization and management processes than its neighbors Kenya and Tanzania, with absence rates of 31% and 13.5%, respectively?
Absenteeism may reflect underlying challenges of low provider motivation, which may be worsened by workload demands. Measuring the average number of outpatient visits seen by a provider per day, caseload per provider is a critically important indicator that can impact wait time for patients as well as overall access to care. From the provider perspective, caseload is a central component of total workload, and for managers is a measure of efficiency and provider effort. A shortage of providers or high absenteeism may cause caseload to rise, potentially compromising service quality and contributing to provider burnout. Conversely, low caseloads may impact provider motivation, absenteeism, and the opportunity to practice skills and procedures, decreasing providers’ overall ability to convert health system inputs into positive health outcomes.
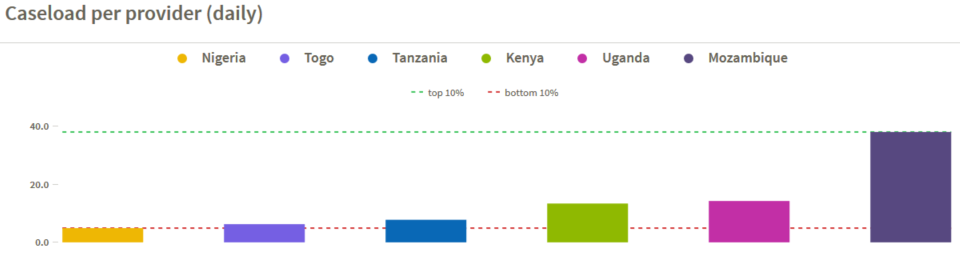
Data reveal wide variation in caseload across countries, ranging from 38.1 daily patients per provider in Mozambique to only 4.9 in Nigeria and raising many questions that warrant deeper diagnosis. For example, is the challenge in Nigeria one of low demand, where patients bypass care at primary level facilities in preference for care at higher level facilities? Or is it one of supply, exacerbated by Nigeria’s relatively high provider absence rate of 32.2%? In Mozambique, are providers able to deliver high quality care, given their relatively high workload?
When health workers are present and seeing patients in facilities, it is crucial to measure the quality of the services they are providing. Diagnostic accuracy is measured by assessing providers’ ability to correctly recognize common tracer conditions in clinical vignettes, including acute diarrhea, pneumonia, diabetes mellitus, pulmonary tuberculosis, and malaria with anemia. Again, the data display significant variation across countries, from 31.6% diagnostic accuracy in Nigeria – implying a high probability that patients will be inaccurately diagnosed and treated, potentially contributing to poor outcomes – to 72.5% in Kenya. Is the variation due to better provider training and ongoing supervision, accessibility of diagnostic tools, a more appropriate daily caseload, or other factors? Furthermore, this is an area where further information would be critical to understand how best to address the issue. For instance, it would be advantageous to know how providers perform in a true clinical setting with the pressures of workload, time constraints, and resource limitations. Once diagnosed, are patients treated correctly?
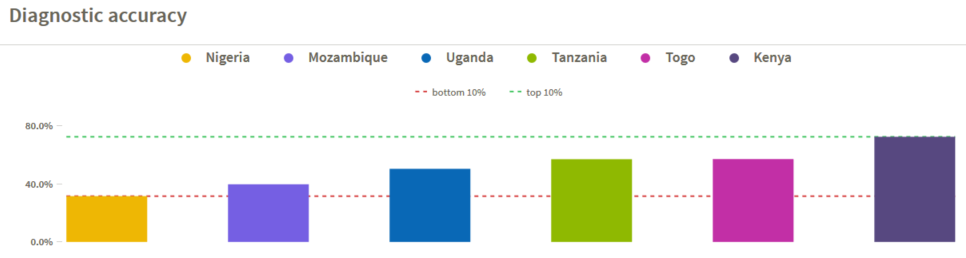
While cross-country comparisons raise important questions, when taken together these indicators can also provide insights into performance variation within countries, indicating areas for improvement. In Togo, providers see few patients per day on average (6.3), are often absent from facilities (35.2%), and are able to accurately diagnose only half of the cases they encounter (57.2%). This suggests that people in Togo may face challenges around the availability of effective PHC services and the organization and management of health services – two important domains of the PHCPI conceptual framework. In contrast, Mozambique experiences relatively low provider absence rates (17.7%) and high daily caseloads (38.1 patients per provider), but has poor diagnostic accuracy at 39.8%. Are providers in Mozambique overworked due to high caseloads, compromising the quality of care, or is more effective supportive supervision needed?
In order to answer such questions, countries need data that are routinely available and comparable within and across countries. We also need to develop new metrics that countries can use to better diagnose challenges and develop effective solutions – for example, measures related to the organization and management of care could help to identify underlying issues leading to high provider absence and poor diagnostic accuracy. Information on the system functions that affect provider knowledge, motivation, and performance will help tailor plans for improvement. With better information on how primary health care services get delivered – and the tools and support necessary to actually use such data for improvement activities – countries and their development partners can understand where change will have the biggest impact and take meaningful steps to improve.
Citations
Education and training. World Health Organization. 2015.
Service Delivery Indicators. World Bank. 2015.
Chloe Lanzara is a Senior Program Associate at Results for Development Institute.
