
Key country characteristics
- Argentina is an upper-middle-income country that covers most of the southern portion of the South American continent
- Population: 46.2M
- GDP Per Capita: $8,441
- Life expectancy at birth: 76

Argentina is a federal country made up of 23 provinces and the city of Buenos Aires and has a population of over 43 million people. There are three types of health care coverage in the country:
In 2004, Plan Nacer was initiated by the National Ministry of Health (NMOH) in Argentina to improve health coverage and outcomes for the public sector in order to meet the morbidity and mortality targets of the Millennium Development Goals. At this time, Argentina had achieved Universal Health Coverage (UHC) in theory, but in practice, effective universal coverage was lacking. This could be seen in the differential outcomes in key health targets such as infant mortality rate between the social security (employed) and public sectors, even though both groups were technically covered equitably.
Plan Nacer was initiated to address this gap in effective coverage of the public sector and align the priorities of and solve agency relationships between the national government and the provinces, and between the provinces and the health facility networks. Plan Nacer was a combination of public insurance strategy and a pay-for-performance scheme. At the outset, Plan Nacer defined three elements of effective coverage: 1) Enrollment; 2) Access; and 3) Quality. Enrollment refers to the active identification of eligible beneficiaries by public sector health providers. This enrollment enables beneficiaries to enroll in explicit health plans and obtain financial protection from healthcare-related costs. However, this first step does not ensure the use of health services; necessitating the addition of the access element, which accounts for the reliable ability to utilize a set of prioritized health services. The third dimension, quality, ensures that the prioritized interventions are provided in a timely fashion and at a level of quality that meets predefined standards.
Plan Nacer, in collaboration with the World Bank Group, identified a set of health service utilization indicators to establish a signal system to ensure effective universal coverage at the national level. The program makes capitated payments to the provinces based on overall results. Sixty percent of the capitated payment is made monthly based on the enrollment of the target population into the program. The additional 40% of the capitation payment is made every four months based on health service utilization indicators called "tracers." These tracer indicators measure the proportion of enrolled patients who received at least one nationally-prioritized health service, or “tracer health service,” over the past four months. Therefore, the capitation payment reflects both enrollment and access. To ensure that the third dimension of effective coverage—quality—is met, payments reflecting access are only made if the received tracer services met the quality standards established in the program’s billing function. Critically, these capitation payments from the national level to the province level are kept in dedicated accounts that get distributed directly to health providers and facilities, which can autonomously determine how to use the funds.
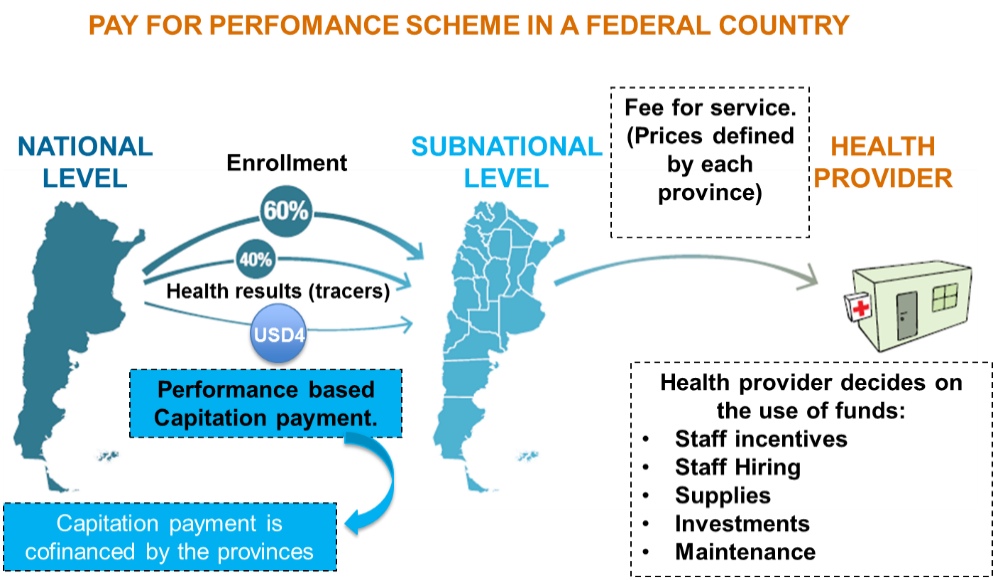
Figure 1: Program Nacer's pay-for-performance scheme between the national and provincial levels. USD: United States Dollars.
Based on the NMOH priority of promoting equity, rollout of Plan Nacer began in 2004 in the Northeast and Northwest provinces, which had the highest mortality rates in the country. Initially, Plan Nacer focused on a defined population of beneficiaries—pregnant women and children under 6 years of age—by identifying 10 tracer maternal and child health services. As described above, provinces were paid based on the number of targeted beneficiaries enrolled and the percent of enrollees who received at least one of these 10 tracer conditions at or above the quality thresholds. Overall, 700,000 beneficiaries were reached in this initial rollout of the program.
Since 2004, Plan Nacer was gradually scaled up to cover the entire public sector of Argentina. In 2007, the program was expanded to include the initial 10 tracer services and accompanying financial structure for the entire country. In 2012, new age groups (children under 11 years of age, adolescents under 19, and women between 20 and 64) were added under the new program name of Programa SUMAR (Figure 2). Finally, in 2015, the program expanded to also include men aged 20-64. With each phase of expansion, the tracer health services were modified based on the covered population’s needs. Since 2015, effective coverage has been measured through the receipt of 14 performance indicators (tracers), as shown in Figure 2.
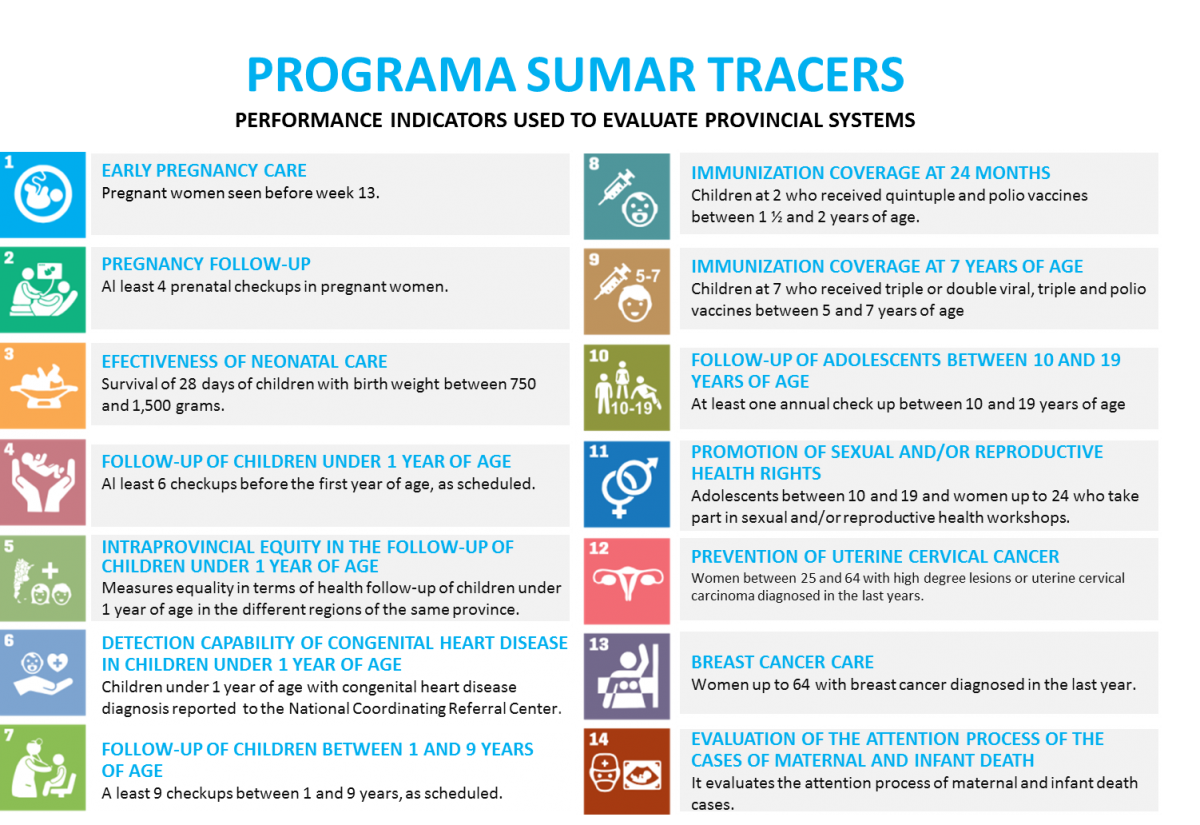
Figure 2: Programa SUMAR performance indicators (tracers)
With each phase of rollout, the implementation team from the NMOH conducted pieces of training and supportive supervision for province health teams to ensure that they could both accurately collect the necessary data and use their results to drive improvements in service delivery. Although the payments and capitation method were the same across all provinces, the implementation team found during the scale-up process that the capacity of each province for using the measurement and improvement tools was varied. As such, the level of support and capacity building required from the NMOH varied accordingly from province to province.
As shown in Figure 3, coverage of Programa SUMAR has increased steadily over time. In this figure, the red line represents the total percentage of the eligible population who has enrolled in Programa SUMAR and received one Basic Health Service, while the green line shows the percent of the eligible population who has received at least one Basic Health Service. The figure shows that, over time, coverage of enrollment and receipt of Basic Health Services has increased. The difference between the red and green lines in this figure also shows the percent of the eligible population who are enrolled but not receiving Basic Health Services.** The shrinking of this gap shows that effective coverage of Programa SUMAR is improving over time. The graph does not include the eligible population of men between 20-64 y.o that were included in Programa SUMAR in April 2015.
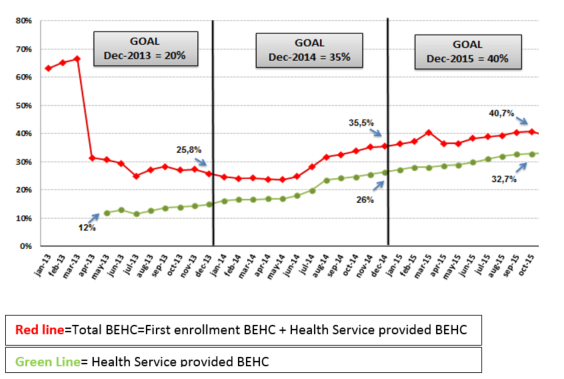
Figure 3: Evolution in the proportion of eligible population with Basic Effective Health Coverage (BEHC) from 2013-2015
In addition to improving coverage and quality, Programa SUMAR has also improved health worker motivation and satisfaction. Although capitation payments make up only an additional 1-2% of the provincial health budgets, this translates into major gains for health facilities and providers and health team motivation has increased since the rollout of the program.1 For example, a survey in the Northeast and Northwest provinces of the country of health facilities found health workers to have a satisfaction level of 7 (on a scale of 10) when asked about the program’s operational design regarding the use of funds at the facility level. The Program sees the motivation of health teams as the main determinant to improving the coverage conditions and quality to which the population has access. Patient satisfaction with care has also improved through the implementation of Plan Nacer/Programa SUMAR. Amongst initial beneficiaries of the program roll-out in the Northeast and Northwest provinces, a study found that patient satisfaction with care increased as the implementation of the program progressed.2
Plan Nacer/Programa SUMAR is one proven example of how pay-for-performance at the facility level can be used to drive improvements in all dimensions of effective coverage, including enrollment, access, and quality. Over the last 12 years of implementation, the project team has learned many generalizable lessons that may prove useful for other countries that would like to replicate such a model. Perhaps most importantly is the lesson that the pay-for-performance program must be designed to reflect the reality of how responsibility and capacity are distributed across the country. Changing the way that data is collected and used is not simple, and ongoing supervision and training need to be tailored to local capacity.
Second, the role of quality monitoring and evaluation (M&E) cannot be overstated. Importantly, the goal of any M&E system must be measurement for improvement, not as an end in and of itself. Reliable baseline data are needed to measure change and understand where to target services, while appropriate indicator selection is critical to ensure that data are methodologically sound, appropriate to the information technology capacity of the country, and have the capacity to demonstrate change over short periods of time. The program’s use of the M&E as a strategic instrument for better implementation has served as a guide for future decisions within an organization that identifies learning as the best prospect of success for effectively promoting its goals.
Finally, the implementation team would stress to anyone embarking on a similar journey to move slowly. Even the 12-year scale-up of Programa SUMAR felt fast to those on the ground implementing, and real change and capacity building takes time.
To learn more about Programa SUMAR, please visit their website here.